In this article, we will be discussing sperm granulomas. Sperm granulomas are inflammatory masses that typically occur following a vasectomy. A vasectomy is a minimally invasive scrotal procedure used for permanent birth control in men. Sperm granuloma is a relatively common complication in men who undergo vasectomy procedures, so we will discuss the pathophysiology of the condition as well as the signs and symptoms men present with. I will also discuss the treatment options for when men develop a symptomatic granuloma.

The Vasectomy Procedure and Vas Deferens
It is helpful to briefly discuss the vasectomy procedure in order to understand the pathophysiology of sperm granulomas. A vasectomy procedure involves a puncture or incision into the scrotum to gain access to the vas deferens or sperm transport tubes.
There is a vas deferens originating from both testicles that will carry sperm via the spermatic cord to the prostate and seminal vesicles located in the pelvis. Most of the semen is produced by the prostate and seminal vesicles, but the sperm is produced by the testicle and transported via the vas deferens.
During a vasectomy, the vas deferens are cut, and a segment is removed for pathologic evaluation. The ends of the vas can be left open, cauterized, or occluded with titanium clips or sutures. Some surgeons also use fascial interposition to separate the two ends in order to reduce the incidence of vasectomy recanalization or failure.
The vasectomy procedure severs the sperm transport tube, which will prevent sperm from reaching the seminal vesicle. Once residual sperm have been cleared from the genital tract, men will develop azoospermia, which means no sperm in the ejaculate. This usually takes about 30 ejaculations and must be confirmed by semen sample.
Vasectomy is the most common surgical procedure performed by urologists, with 500,000 procedures performed annually in the general population.
Vasectomies have a relatively low complication rate, but some men can experience pain and swelling of the testicles for a few days. Other complications include bleeding, infection, and chronic nerve pain.

Pathophysiology of Sperm Granuloma
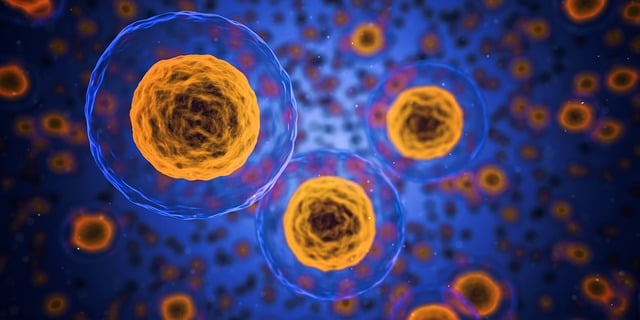
After the vas deferens are cut during a vasectomy, it’s possible that sperm leaks into the surrounding tissues. This is more likely to occur when the ends of the vas deferens are left open. This extravasated sperm can lead to a foreign body inflammatory response. The extravasated sperm are essentially seen as “foreign” by the immune system.
The Blood-Testicle Barrier
Due to the blood-testicle barrier, extravasated sperm are seen as foreign invaders by our immune cells. These immune cells include macrophages and lymphocytes, which release inflammatory cytokines to attack the sperm leaking into surrounding tissue. This is the immune system’s reaction to a bacteria or virus. Our immune system sees our sperm cells as foreign and will form anti-sperm antibodies to those sperm once they violate the blood-testicle barrier.
The chronic inflammation leads to a foreign body giant cell reaction and inflammatory mass. Eventually, the inflammation leads to fibroblast infiltration and fibrosis, resulting in a mature granuloma. When a sperm granuloma is surgically removed, histological examination will reveal a central mass of sperm cells surrounded by inflammatory cells and fibrous tissue.
Epididymal Sperm Granuloma
The same process can occur in the epididymal epithelium following vasectomy procedures. When the vas deferens is occluded during surgery, pressure within the epididymis can develop due to fluid buildup driving sperm cells into the epididymal epithelium. This leads to the same granulomatous inflammatory response described above. Sperm granulomas in the epididymis can lead to obstruction.
Therefore, sperm granulomas can appear at the ends of the vas or in the epididymis post-vasectomy.
Clinical Presentation of Sperm Granulomas
Sperm granulomas may develop in up to 40% of men who undergo a vasectomy. Most are asymptomatic, meaning they do not cause pain or discomfort. Typically, they are quite small, in the neighborhood of 1 cm in size. Sometimes, they are noticed by a sexual partner. In rare cases, they can be larger in size and cause symptoms.
Sperm granulomas can present with symptoms as early as a few days following a vasectomy, but a fully developed sperm granuloma may take months to mature.
Upon physical exam of the scrotum, men will often notice a small nodule and present it to their urologist. The nodule can occur at the vasectomy site or in the epididymis. If the granuloma is asymptomatic, patient education is all that is required.
Sperm granulomas can cause pain in some cases. Pain symptoms can be a localized ache, sharp pain, or generalized scrotal discomfort. The pain can radiate to the groin or flank. In some cases, the pain can be colicky and cause kidney spasms. Some men will report worsening pain symptoms with heavy lifting or strenuous exercise. Rarely, chronic pain may develop.
Diagnosis of Sperm Granuloma
The diagnosis of sperm granuloma begins with a careful surgical history because, more often than not, it will follow a vasectomy. However, a history of other scrotal procedures, as well as scrotal trauma, should be discussed. A history of scrotal infections must also be elucidated, including previous sexually transmitted infections.
Physical examination by a urologist will usually reveal a small mass in the spermatic cord or epididymis. The small lump will usually be in the neighborhood of 1 cm in size, although I have seen a case report of a sperm granuloma that was 4 cm in size. The granuloma may be tender to palpation.

Differential Diagnosis
The differential diagnosis of a scrotal mass is quite extensive. While a sperm granuloma may be suspected based on surgical history and mass location, other scrotal pathology is certainly in the differential diagnosis.
Other causes of scrotal masses include abscesses, sexually transmitted diseases, epididymal cysts, hernias, testicular tumors, and lipoma of the spermatic cord. Physical examination alone may not be enough to distinguish these entities.
Urology case reports have also demonstrated a large sperm granuloma that was mistakenly diagnosed as a supernumerary testis.
Diagnostic Testing
The most common diagnostic imaging study performed for a scrotal mass or vasectomy-related pain is a scrotal ultrasound. Ultrasound can usually distinguish between solid and cystic masses. It also can identify increased blood flow when Doppler technology is used. Increased vascular flow to a mass may indicate underlying inflammation or tumor.
More sophisticated imaging may be done with magnetic resonance imaging (MRI) in rare cases. MRI has a much higher resolution than ultrasound but is more costly.
If infection is suspected, urine and blood testing may be performed. If sexually transmitted infections are a concern, your urologist will order appropriate lab testing.

Pathologic Evaluation
A definitive diagnosis of sperm granuloma can only be made by pathologic evaluation following surgical removal of the mass. Histologic findings are described earlier in the article.
Clinical Implications of Sperm Granuloma
Most sperm granulomas are small and asymptomatic, requiring no treatment. Some urologists believe that a sperm granuloma is protective by safeguarding the testicle and epididymis against obstruction. This is why some surgeons advocate for leaving the vas tubes open during a vasectomy.
Sperm granulomas have been implicated in vasectomy failures. Microtubules can form within a sperm granuloma and increase the likelihood that recanalization of the two vassal ends will occur. Recanalization leads to vasectomy failure in approximately 1 in 2000 surgical procedures. While vasectomies can fail, no form of birth control can prevent pregnancy more effectively.

Surgeons who use mucosal electrocauterization and careful distal occlusion to avoid necrosis of the basal stumps will see a lower incidence of sperm granuloma. I perform vasectomies in this manner because I believe it reduces the risk of vasectomy failure and chronic pain.
Sperm Granulomas and Vasectomy Reversal
A vasectomy is considered permanent birth control, although a small percentage of men will regret their decision and elect to have a vasectomy reversal. Vasectomy reversals are performed by fellowship-trained urologists using microsurgery.

Vasectomy reversal is a complex procedure where the distal vassal segment is reattached to the proximal stump if sperm quality is good at the proximal end. If few sperm cells are seen at the time of surgery, an epididymo-vasotomy may be performed. The distal end of the vas is mobilized and connected to an epididymal tubule directly.
Sperm granulomas seem to increase the likelihood that healthy sperm cells will be found during vasectomy reversal. Finding a sperm granuloma at the vasectomy site also increases the success rate of vasectomy reversal. The most likely cause for this increased fertility is that sperm granuloma prevents dilation and scarring of the epididymal tubules.
Only 2% of men regret their decision to have a vasectomy, so the benefits of sperm granuloma in this scenario are not far-reaching.
Post Vasectomy Pain Syndrome (PVPS)
PVPS is a pain syndrome that develops following a vasectomy procedure. Sperm granulomas have been implicated in PVPS. PVPS is usually defined by persistent scrotal pain that fails to resolve within six months of vasectomy.
PVPS is a devastating consequence of vasectomy because it can be very difficult to treat and can lead to depression and low sex drive. Anti-inflammatory medications, local anesthesia, and steroid injections are often used to treat PVPS. Severe cases may require narcotic pain medications or surgical intervention.
If pain is localized to a sperm granuloma, surgical removal may resolve the issue. The granuloma causing pain is excised, and the mucosal ends of the vas deference are cauterized, preventing recurrence.
Preventing a Sperm Granuloma
As discussed above, surgical techniques can reduce the risk of sperm granulomas. Men undergoing a vasectomy should also be instructed to abstain from ejaculation for seven days following surgery to reduce the risk of sperm granulomas.
Treatment Options
Treatment is indicated to alleviate pain when sperm granulomas are symptomatic and will vary depending on severity. Treatment options include conservative measures, including scrotal support using a jockstrap and ice packs. An ice pack can relieve pain and swelling immediately following a vasectomy, but sperm granulomas typically present weeks later when no swelling is present. Warm baths can sometimes help symptoms.
Treatment May Require Pain Medications
Anti-inflammatory medications and pain medications are sometimes needed if pain is substantial. Local anesthetics and steroids can be injected into the area of the sperm granuloma when oral pain medication fails.

Profound cases of pain that fail conservative measures may require surgical excision of the sperm granuloma. This is a relatively minor procedure but does require general anesthesia. A small incision is made in the scrotum, and the sperm granuloma is isolated. The mass is excised, and the vas deferens are cauterized to prevent recurrence.

Conclusions
Sperm granulomas occur in up to 40% of men who undergo a vasectomy. Surgical techniques can determine the likelihood of developing a sperm granuloma. Most sperm granulomas are asymptomatic, and the best course of action is observation. Sperm granulomas have been implicated in vasectomy failure and PVPS.
A small percentage of sperm granulomas will cause pain and require treatment. Various treatment options are available ranging from oral medication, local injections and surgery. A urologist who specializes in vasectomy and/or vasectomy reversal will be well-versed in the treatment of sperm granuloma.
