Testosterone deficiency or low testosterone
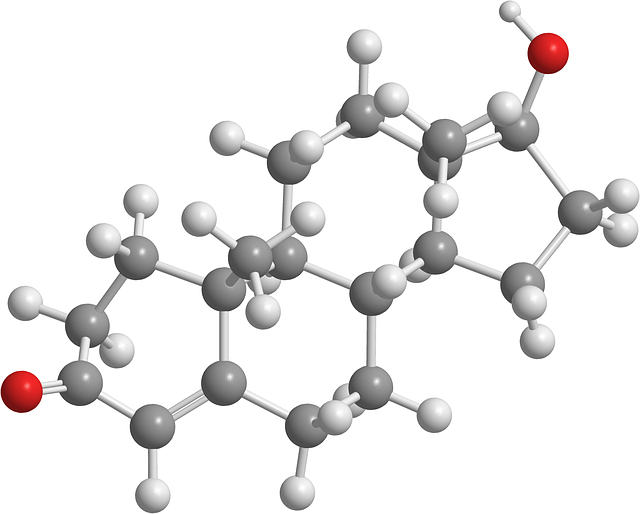
Testosterone deficiency or hypogonadism is a condition in men caused by inadequate testosterone production. Testosterone is the most important male sex hormone or androgen in the body. The majority of testosterone is produced by the Leydig cells of the testicle while a very small amount is manufactured by the adrenal glands.
Low testosterone (low T) symptoms
Symptoms of low T include low libido or decreased sex drive, erectile dysfunction, fatigue or reduced energy levels, lack of motivation, insomnia, weight gain and difficulty building muscle mass.
Hypogonadism can also lead to adverse health consequences including low sperm counts, insulin resistance, reduced bone density and metabolic syndrome. Bottom line testosterone is a vital hormone in men.
Diagnostic considerations
Blood tests can be ordered by your physician to assess testosterone in your blood or serum. If serum testosterone levels are low a search must ensue for underlying causes such as hypothyroidism, pituitary gland disorders and hemochromatosis. Certain medications and illicit drugs can also affect testosterone production.
If a correctable underlying etiology is not identified treatment of low testosterone will require some form of testosterone replacement therapy to restore normal testosterone levels. Testosterone replacement therapy may involve exogenous testosterone or medications that increase endogenous testosterone production. Once normal total testosterone levels are achieved with therapy most men will experience marked improvement in their symptoms.
Certain conditions must be excluded at the time of diagnosis before starting a patient on testosterone replacement therapy. These conditions include breast cancer, sleep apnea and prostate cancer. Prostate cancer screening requires a digital rectal exam (DRE) and PSA blood test. Normal levels of red blood cells and lipids should also be present before starting someone on hormonal therapy.
Side effects of testosterone replacement therapy
Like all drugs and hormones, testosterone therapy has potential side effects and may even be dangerous in certain high risk groups such as men suspected of having prostate cancer. Close supervision by an experienced urologist is required to keep therapy safe and effective.
Serial physical examinations must be performed, men must be questioned about potential side effects and the healthcare provider must order blood tests to include measurement of hematocrit (# of red blood cells) and prostate specific antigen.
Too much testosterone must also be avoided since supraphysiologic testosterone levels carry a higher risk of side effects. Supraphysiologic testosterone levels are seen in men taking anabolic steroids. High testosterone may increase the risk of prostate cancer. Men with prostate cancer can cause their prostate cancer to spread by taking excess testosterone.

Laboratory testing in men with low testosterone
The laboratory diagnosis of low testosterone can be complex and confusing to patients so I am going to unpack this topic in detail. The most common blood test ordered to assess testosterone is a total testosterone level with a normal reference range of 300-1,000 ng/dL. When most doctors refer to obtaining a “testosterone test” they mean to test total testosterone. Other testosterone measurements can also be done to assess free and bioavailable testosterone.
Testosterone assay complexity
A multitude of assays are used in laboratories to measure hormone levels. GC-MS or gas chromatography-mass spectrometry and LC-MS/MS or liquid chromatography-tandem mass spectrometry are just two techniques used at major laboratories to measure total testosterone. Direct, analogue immunoassay is one technique used to measure free testosterone by some lab companies. Immunological and mass spectrometric techniques can be used to measure sex hormone binding globulin, a protein that tightly binds testosterone making it less bioavailable.
The laboratory techniques to measure male hormones are numerous and they each have limitations and short falls. The important thing is that your healthcare provider is well versed in the different techniques and standards being used by the lab companies they trust to measure testosterone levels in their patients. This requires a firm knowledge of biochemistry and sometimes discussions with lab personnel. Urologists who specialize in andrology will have this deep understanding to help facilitate the proper diagnosis of low testosterone in men. Urologists are also sexual medicine experts.

Total testosterone
A serum total testosterone level is the most common blood test used in medicine to diagnose men with low testosterone. As the name implies, total testosterone measures ALL of the testosterone present in the serum or blood. Some of the testosterone in our blood is bound to proteins and some is free and unbound. Total testosterone measures all of it including free testosterone.
What is normal
Normal total testosterone according to most laboratory reference ranges is 300-1,000 ng/dL although I consider a normal total testosterone to reach a level of 1,200 ng/dL. The best time of day to measure testosterone is in the morning (between 8-11 AM) because of the diurnal variation in testosterone production. Normally testosterone secretion peaks in the morning and falls in the afternoon and evening hours. Measuring it in the morning is key to an accurate diagnosis.
AUA and endocrine society guidelines
The American Urologic Association and endocrine society consider the diagnosis of low testosterone to be made when two morning total testosterone values are below 300 ng/dL. There is not total agreement on this cutoff within the global medical community. In Europe, for example, a cutoff of 350 ng/dL is used.
Men with symptoms of low testosterone and two total testosterone levels below 300 ng/dL meet the most strict definition of low testosterone in the United States. However, some men with total testosterone levels above 300 ng/dL may still warrant replacement therapy.
Sex hormone binding globulin (SHBG)
Sex hormone binding globulin is a protein made in the liver. SHBG enters the blood stream and tightly binds testosterone. SHBG also binds to two other sex hormones, dihydrotestosterone and estrogen. When total testosterone is measured it includes the testosterone bound to SHBG. The testosterone bound to SHBG is trapped in the blood because the bond between SHBG and testosterone is very powerful.
SHBG-bound testosterone is not able to leave the blood stream and enter tissues to exert it’s effect. Normal SHBG levels range between 10-50 nmol/L. Certain conditions including hepatitis and hyperthyroidism can increase SHBG levels. Certain medications may increase SHBG levels. When SHBG levels exceed the normal range, a larger portion of testosterone will be trapped in the blood stream.
Obesity, type 2 diabetes mellitus and hypothyroidism lower SHBG production. This is one of the reasons a comprehensive lab evaluation is required to accurately assess a patient with testosterone deficiency. Low concentrations of total testosterone and SHBG levels are correlated with an increased risk of metabolic syndrome.

Other proteins that bind sex hormones
Sex hormone binding globulin is not the only protein in the blood that binds the sex hormones: testosterone, dihydrotestosterone and estradiol. Testosterone is also bound to serum albumin. Albumin is a copious protein found in the blood. Produced by the liver it helps maintain fluid balance in the body by keeping water in the blood so it doesn’t leak into tissues.
Albumin bound testosterone is not a tight chemical bond so albumin can transport testosterone in the blood and release it to tissues. Albumin also transports other hormones, vitamins and enzymes.
Testosterone also binds to corticosteroid binding globulin (CBG) and orosomucoid but it’s relationship to these proteins and how they modulate bioavailable testosterone levels is poorly understood.
Free testosterone
Free testosterone is the fraction of total testosterone unbound to proteins in the serum. Normal free testosterone levels range between 50-250 pg/mL and make up between 2-3% of total testosterone. Low free testosterone levels are indicative of clinically significant hypogonadism.
Free testosterone is capable of freely leaving the blood and entering tissues such as the brain, penis, adipose tissue and muscle. Free testosterone can easily bind to the androgen receptor. This hormone-receptor complex can enter the nucleus and alter gene transcription leading to changes in physiology.
Testing free testosterone levels is considered by some to be a better approach to diagnosing men with testosterone deficiency since it may more closely reflects usable testosterone.
Methods for measuring free testosterone are often imprecise. Reliable assays are not always available to clinicians. Algorithms using SHBG binding levels can be used to estimate free testosterone levels in the body.
What is considered low free testosterone?
As mentioned earlier, free testosterone measurements can be fraught with technical challenges and imprecise results. Algorithms that use the binding properties of testosterone to albumin and SHBG are probably more accurate in most instances.
Having said that, free testosterone levels should be in the accepted normal reference range of a reputable laboratory. Free testosterone levels range between 50-250 pg/mL in most labs. If low free testosterone levels (less than 50 pg/mL) are present on a blood test, it usually indicates a deficiency in the body’s usable or bioavailable testosterone.
In my practice, I don’t find free testosterone to be very helpful in the diagnostic process unless total testosterone levels are in the normal range. If total testosterone levels are low, I base my treatment decisions on that information with rare exceptions.
If total testosterone levels are in the normal range but free testosterone levels are low, the diagnosis of testosterone deficiency is highly likely. Most men with normal total testosterone levels and low free testosterone will respond to testosterone replacement therapy.
Bioavailable testosterone
Bioavailable testosterone is the term used to describe the testosterone in the blood that is actually usable by tissues. In theory, bioavailable testosterone is what we truly want to understand in men experiencing symptoms of low testosterone.
Testosterone exists in both bound and free forms within the serum. Proteins that bind testosterone include SHBG, albumin and corticosteroid binding globulin. The only protein that has a very high affinity for testosterone is SHBG. Testosterone attached to albumin is a low affinity relationship so testosterone can hop off the albumin molecule with ease.
Bioavailable testosterone measurements are therefore the testosterone attached to albumin plus free testosterone in the blood. Total testosterone minus SHBG bound testosterone is called bioavailable testosterone.
Total testosterone = SHBG-T + albumin-T + free testosterone
Bioavailable testosterone levels= total testosterone – SHBG-T
In most clinical laboratories, when bioavailable testosterone levels are ordered it is not actually measured directly. Rather, it is calculated by measuring total testosterone, SHBG and albumin and using equilibrium binding constants of testosterone to these proteins.
The pituitary gland and the testicle
The pituitary gland is the master gland that sits at the base of the brain. The pituitary gland secretes two hormones that impact testicular function. These hormones are luteinizing hormone (LH) and follicle stimulating hormone (FSH). Gonadotropin releasing hormone is produced by the hypothalamus to stimulate the production of luteinizing hormone LH and FSH
Luteinizing hormone works on the Leydig cells of the testicle to stimulate testosterone secretion while follicle stimulating hormone acts on the Sertoli cells of the testicle to promote a healthy sperm count.
Men with symptoms of low testosterone and high LH levels have primary hypogonadism which indicates testicular failure. Low testosterone levels and low LH levels indicate secondary hypogonadism or hypogonadotropic hypogonadism where the problem lies within the pituitary gland, not the testicle.
Men with low normal testosterone levels but high normal or mildly elevated LH levels may be more likely to benefit from testosterone therapy in my experience. So, properly measuring free and bioavailable testosterone levels as well as pituitary hormones can be helpful in borderline cases.

Estrogens in men
When discussing total and free testosterone levels in men we also must consider the importance of estrogens in male physiology. Estrogens have historically been considered a female hormone and they were believed to counteract the effects of testosterone in men. This turned out to be untrue.
Estrogens serve a vital role in men, as they do in women. Ovarian conditions such as polycystic ovarian disease can wreak havoc on female physiology. Estrogen receptors are found in a variety of tissues including the brain, penis, muscles and bones in men. Estrogen promotes a healthy mood, bone and cardiac health and actually can help promote muscle mass.
Testosterone is produced by the Leydig cells of the testicle. As it circulates in the blood stream some of our testosterone makes it’s way into the adipose tissues. Here an enzyme called aromatase converts a small amount of testosterone into estradiol, the primary estrogen in men.
Estradiol can reenter the circulation and travel throughout the body to modulate function through its binding to the estrogen receptor. Normal estradiol levels in men range between 10-42 pg/mL in most laboratories. Too much testosterone can lead to elevated estradiol levels which may cause male breast enlargement.
Elevated estrogens and negative feedback
Elevated estradiol levels can be seen in men with high aromatase activity. This can occur in men with significant belly fat. Estrogens should be measured on a blood test in men who are being investigated for low T symptoms. In rare case, adrenal gland tumors can produce high levels of estrogens. High testosterone levels can also indicate both adrenal gland and testicular tumors in men.
Estrogens also play a key role in the negative feedback exerted on the pituitary gland to maintain the correct balance of sex hormones in the body. Estrogens decrease the release of luteinizing hormone and follicle stimulating hormone FSH from the pituitary gland.
Treatment of elevated estradiol
Some men may develop elevated levels of estradiol while on therapy for low free testosterone levels. This can lead to adverse health consequences and side effects such as fluid retention and gynecomastia. Elevated estradiol levels can be managed with medications that inhibit the aromatase enzyme. Aromatase inhibitors such as anastrozole will lower estradiol levels and raise total and free testosterone levels.
Mildly elevated estrogens do not require treatment when men are using synthetic testosterone for the treatment of low testosterone. A good clinician will also consider the testosterone to estradiol ratio when making treatment considerations for low testosterone.
Driving estrogens too low
A common problem I have seen over the years when men are not being treated by an expert physician is low estradiol. Men treated by low T clinics are often given aromatase inhibitors they don’t need. Since estrogens are actually important for male physiology, normal levels must be maintained.
If estradiol levels are lowered too much men can experience serious side effects such as low sex drive, depression, loss of muscle mass and hot flashes. I’ve actually seen men experience the symptoms of menopause when overtreated with anastrozole.
Clinical endocrinology
As you can see, the laboratory diagnosis of decreased testosterone is complex. The most common test performed by a healthcare provider to assess symptoms of low testosterone is a simple testosterone measurement. This is typically a measurement to test total testosterone levels. Most experts recommend at least two total testosterone measurements on separate days in the morning hours. If both total testosterone levels are low the diagnosis is pretty clear cut. If not, further assessment of free testosterone is warranted.

When total testosterone levels are normal
If total testosterone is normal in adult males complaining of low testosterone symptoms further testing free testosterone levels is the next step. Men with low free testosterone should be treated if no contraindications are present. Some experts may assess total and free testosterone levels initially. But men with apparently adequate total testosterone values should definitely have free testosterone levels measured.
Depending on the local laboratories available, a physician may also asses bioavailable testosterone levels in men with normal free testosterone levels. Measurement of free and bioavailable testosterone can often be helpful in men with normal total testosterone.
Furthermore, assessment of pituitary hormones and estradiol levels can also be used to help physicians understand free and bioavailable testosterone measurements.
Putting it all together
Expert clinicians will use complex laboratory testing, assessment of symptoms as well as physical examination findings to make an accurate diagnosis of hypogonadism. It’s not as simple as drawing a blood test or two.
The symptoms of low testosterone (also referred to as late onset hypogonadism) may include fatigue, low sex drive, erectile dysfunction, depressed mood and difficulty building muscle mass.
Urologists need a deep understanding of symptomatology and must perform a careful physical examination when dealing with men complaining of low T symptoms. Some men with low testosterone will have characteristic physical exam findings such as reduced body hair, testicular atrophy and gynecomastia.
Doctors will then perform a full laboratory assessment that may include a variety of testosterone blood tests including free testosterone, SHBG, bioavailable testosterone, estradiol and pituitary hormones.
Other causes of symptomatology must also be excluded. Once an accurate diagnosis is made through history, physical exam and lab testing medical contraindications must be excluded. These include untreated sleep apnea, breast mass, prostate exam abnormality, uncontrolled dyslipidemia and hypertension as well as elevated red blood counts.
Treatment
If no medical contraindications are present testosterone treatment should be offered. There are a variety of treatment options available including oral testosterone, topical gels/creams, injectable testosterone and implantable testosterone pellets.
Men should avoid gimmicks such as “bioavailable testosterone” and seek out a urologist using FDA approved testosterone formulations.
Men started on testosterone replacement therapy must be monitored closely. This includes a frequent assessment of clinical benefits and potential side effects. The resolution of symptoms in men taking testosterone can be just as important as the lab tests when confirming the accurate diagnosis of hypogonadism.

Clinical follow-up
Meticulous clinical follow-up is required to keep testosterone therapy safe and effective. This includes at the very least annual physical examination to assess things such as blood pressure, body composition, testicular atrophy and to exclude breast and prostate masses.
Laboratory testing every 6 months is the bare minimum and must include hematocrit and prostate specific antigen. Annually, I like to assess lipids, hemoglobin A1c and other metabolic biomarkers of disease.
