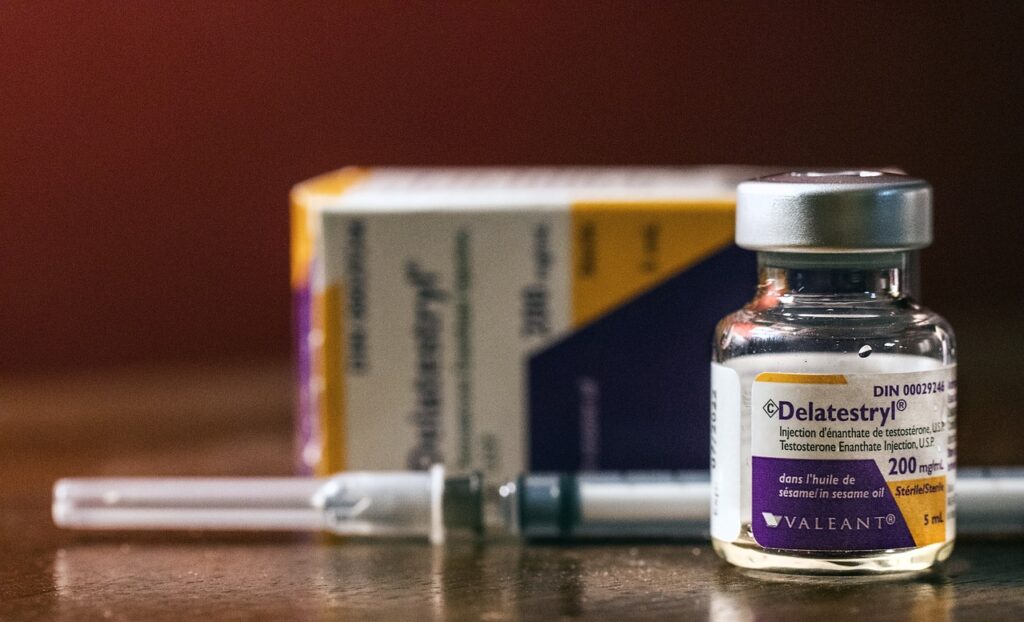
In this article, I will be discussing prescribed medication that lower testosterone levels in men and how to clinically diagnose and treat the issue effectively.
Testosterone and Low T Symptoms?
Testosterone is the quintessential androgen or male hormone in the human body. Normal levels of testosterone are required in both men and women for normal physiology. Low levels of testosterone in men can cause a multitude of symptoms including low sex drive, erectile dysfunction, fatigue, lack of motivation, insomnia, irritability, increased fat distribution and reduced exercise tolerance. Low levels of testosterone can also put men at risk for depression, insulin resistance, reduced muscle mass, metabolic syndrome and osteoporosis.
Medical Conditions that Lower Testosterone
A variety of medical conditions can impair testosterone production and lead to hypogonadism including pituitary gland disorders, testicular dysfunction, hemochromatosis, obstructive sleep apnea and hypothyroidism.
Medications that Lower Testosterone Levels
Research has shown that certain medications cause low testosterone as well. A variety of medication classes including but not limited to statins, antidepressants, chemotherapeutics, opioids, antifungals and certain hypertension medications can lower testosterone levels. Most of these drugs are prescription medications but there are some over-the-counter drugs which can potentially lead to decreased testosterone levels.
Alcohol, marijuana and other illicit drugs may also have a negative impact on levels of testosterone.
Testosterone Endocrinology
Testosterone physiology is complex but we will take a deep dive into the topic. We have to understand testosterone works in the human body if we truly want to comprehend how certain prescription medications impact testosterone levels. We will also discuss how testosterone deficiency is diagnosed and what is considered normal levels of testosterone.
Once we have a solid understanding of testosterone endocrinology we will talk about specific over-the-counter and prescription medications and how they impact testosterone production. Finally, we will address the clinical implications of this information should you need to continue medications that adversely effect testosterone levels.
Testicular Physiology 101
The functional testicle is comprised of two cell types: Sertoli and Leydig cells. Leydig cells are the testosterone producing cells of the testicle while Sertoli cells handle fertility. Leydig cells take cholesterol and produce testosterone through a series of complex steroidogenic enzymatic reactions.
Cholesterol can be synthesized by the Leydig cell itself or extracted from circulating lipoproteins in order to produce testosterone. Prescription medications that lower cholesterol theoretically may affect testosterone production and we will discuss this when we address the statins. Other medications that interfere with cholesterol metabolism may also impact testosterone biosynthesis.
The Hypothalamic-Pituitary-Testicular Axis
All glands, including the testicle, are controlled by the pituitary gland which sits at the base of the brain. The pituitary gland is called the “master gland” and is heavily influenced by the hypothalamus. The hypothalamus secretes gonadotropin releasing hormone (GnRH or LHRH) in a pulsatile manner which causes the pituitary gland to release luteinizing hormone (LH). The key to this relationship is that the LHRH stimulation must be pulsatile, not continuous.
LH travels to the testicle and stimulates the Leydig cells to begin the steroidogenic enzymatic reactions that lead to the production of testosterone.
Small amounts of testosterone are converted to other hormones including dihydrotestosterone (DHT) and estradiol. Estradiol exerts a negative feedback effect on the hypothalamus and pituitary gland. Estradiol reduces LHRH secretion by the hypothalamus and LH secretion by the pituitary gland thereby lowering testosterone biosynthesis.
Testosterone and Dihydrotestosterone
A small amount of testosterone is converted into dihydrotestosterone (DHT) by an enzyme called 5-alpha reductase. 5-alpha reductase is primary located in the prostate, skin and liver. DHT is a very potent androgen involved in sexual differentiation of the fetus and young males. In adult males, DHT is primarily involved in prostate growth and hair loss.
Inhibitors of 5-Alpha Reductase
Medications that inhibit 5-alpha reductase include finasteride and dutasteride. These medications increase testosterone levels and decrease levels of DHT in the blood, hair follicle and prostate. Reducing DHT levels can slow male pattern baldness and treat the symptoms of prostate enlargement.
DHT is eventually broken down into metabolites including some neuro-steroids. Medications that inhibit 5-alpha reductase have been associated with sexual and psychological side effects that may persist after drug cessation. Men taking these medications can develop this post-finasteride syndrome, the underlying mechanism of which is poorly understood. It likely has something to do with the downregulation of neuro-steroid metabolites.
Testosterone and Estradiol
A small portion of testosterone is converted into estradiol by an enzyme called aromatase. Aromatase is primarily located in adipose tissue. Estradiol is an important hormone in both men and women. Some of the benefits men experience when prescribed testosterone therapy actually come from the increase in estrogen levels.
Estrogen and Negative Feedback
Estradiol also serves a vital role in the negative feedback of the hypothalamic-pituitary-testicular axis. Selective estrogen receptor modulators like clomiphene block the estrogen receptor at the level of the pituitary gland which increases LH levels leading to more testosterone production. Clomiphene is a drug used to treat infertility in men and women. It can also be used to treat low testosterone levels in men who wish to maintain fertility.
Any medication that increases aromatase activity would lower testosterone levels and raise estradiol. Excessive levels of estradiol in men can lead to symptoms consistent with a low testosterone state.
Normal Testosterone Levels
The most common measurement of testosterone is a total testosterone level. It is fairly easy to measure and the common assays used by major laboratories are accurate. A normal total testosterone level is between 300-1,000 ng/dL.
SHBG, Free and Bioavailable Testosterone
A large component of testosterone in the blood is bound to proteins including albumin and sex hormone binding globulin (SHBG). A small fraction of testosterone is free or unbound. The bond between testosterone and SHBG is very tight while the albumin-testosterone bond is weak.
Testosterone bound to SHBG is essentially unusable by the body because it is trapped in the blood stream. Albumin bound testosterone and unbound testosterone can leave the blood stream and enter tissues to exert their effects. This fraction of testosterone is called bioavailable testosterone.
Free and bioavailable hormone levels can be measured but the assays are more complex and some yield inconsistent results.
Medications can Alter Sex Hormone Binding Globulin (SHBG)
Certain medical conditions and drugs can alter SHBG levels in the blood. If a drug increases SHBG levels it will lower the bioavailable testosterone in the body, potentially causing a deficiency in usable androgen. Metformin and certain anticonvulsants are just a few drugs that increase SHBG levels therefore lowering free androgen.
Understanding the complex assays used to measure these biomarkers and their normal reference ranges is unnecessary for our discussion on drugs that lower hormone levels.
The Androgen Receptor
When testosterone is able to leave the blood stream and enter tissues it must bind to the androgen receptor (AR) located in the cytosol of the cell. Once bound, the testosterone-AR complex enters the nucleus and alters gene transcription.
Gene transcription produces messenger RNA (mRNA) which undergoes translation into proteins by the ribosome. Proteins can change cellular and tissue function.
Androgen Receptor Inhibitors
Drugs that block the binding of testosterone to the androgen receptor will create a biochemical state of testosterone deficiency even though androgen levels are maintained.
Summarizing Testosterone Physiology
Under pulsatile secretion of LHRH, the pituitary gland secretes LH leading to increased production of testosterone by the Leydig cells of the testicle. Testosterone enters the blood stream where much of it is bound to proteins including SHBG. Bioavailable testosterone is free to enter tissues and exert it’s effect.
A small amount of testosterone is converted into DHT by 5-alpha reductase. Estradiol is produced from the aromatization of testosterone by the enzyme aromatase. While estradiol is important for a variety of tissues, it serves as a negative feedback hormone at the level of the pituitary and hypothalamus to reduce testosterone production.
Testosterone must bind to the androgen receptor in order to exert it’s powerful effects on tissues.
Prescription medications or other medications that interfere with this complex interplay of hormones, blood proteins and receptors can cause a state of low testosterone.
Prescription Medications that Cause a Quantitative or Qualitative Low T State
As mentioned earlier, several classes of medications can lower testosterone levels through a variety of mechanisms. Now that we understand testosterone physiology we can take a deeper dive into particular medication classes to see how they impact androgen biochemistry.
Mechanisms by which Drugs Lower Testosterone Levels
Medications decrease testosterone biosynthesis through different mechanisms. Other medications may increase SHBG levels which reduces bioavailable testosterone. A few medications block the androgen receptor essentially yielding a low testosterone state while maintaining normal serum levels of testosterone.
Some medication effects on testosterone are poorly understood and not all medication that lower testosterone cause clinical detriment. Some medications may impair testosterone physiology by more than one mechanism. For example, some prescription medications may decrease testosterone biosynthesis and also work as an antiandrogen at the receptor level.
After we review the different drug classes and what we know about their negative effects on testosterone we will address the clinical implications for the management of the low T patient.
LHRH Agonists and Antagonists
As discussed, the hypothalamus secretes LHRH in a pulsatile manner. This pulsatile exposure of LHRH to the pituitary circulation causes LH to be secreted by the pituitary gland. LH is the chemical signal to the Leydig cells of the testicle to increase the production of testosterone.
LHRH antagonists are medications that block the LHRH receptor in the pituitary gland. This shuts down LH production by the pituitary which essentially flips a switch and turns off the testicle. LHRH agonists are drugs that biochemically mimic LHRH. When administered to men these medications initially increase testosterone production. However, when given continuously the normal physiologic pulsatile exposure to LHRH is lost leading to a shut down of pituitary LH secretion.
Chemical Castration
These two types of prescription medications yield castrate levels of testosterone (less than 25 ng/dL). Why would we want to chemically castrate men? The answer is prostate cancer. In the 1960’s, Charles Huggins discovered that surgically castrating men with metastatic prostate cancer put their cancer into remission. He won the Nobel Prize for this discovery and it drastically changed the management of advanced prostate cancer forever.
Treatment of Advanced Prostate Cancer with LHRH agonists
LHRH agonists and antagonists were developed to treat metastatic and locally advanced prostate cancer in lieu of surgical castration. While these drugs are very effective at lowering testosterone levels and treating prostate cancer they come with a substantial side effect profile. Men taking these drugs basically experience profound symptoms of low testosterone. Researchers have also shown that these men are at risk for cardiovascular disease, reduced bone mass, abnormal fat distribution, reduced muscle mass and dementia.
Androgen Receptor Blockers
The gold standard for treating men with advanced prostate cancer who require chemical castration is the LHRH agonists just discussed. However, the adrenal glands produce small amounts of androgens that may stimulate the androgen receptor causing cancer proliferation. Drugs that block the androgen receptor can prevent these androgenic effects and may be combined with LHRH agonists/antagonists.
In some men with prostate cancer, monotherapy with androgen receptor blockers is sometimes utilized without LHRH agonists/antagonists. Treating men with androgen receptor blockers will create a low testosterone state while maintaining normal testosterone levels. While there may be some benefits to androgen receptor blocker monotherapy compared to LHRH agonists, cancer control is generally not as good.
Imidazole Antifungals
Ketoconazole is the classic imidazole antifungal agent mentioned when discussing low testosterone levels. Ketoconazole inhibits a cytochrome P450 enzyme in fungi responsible for producing the phospholipids necessary to maintain the integrity of the cell membrane. If the fungus can’t maintain a healthy cell membrane it dies. Ketoconazole is used to treat both skin and systemic fungal infections.
Ketoconazole Induced Hypogonadism
Ketoconazole also inhibits steroidogenic enzymes in the testicle and adrenal gland responsible for androgen biosynthesis. High dose ketoconazole induces a rapid and drastic reduction of serum testosterone to castrate levels. In fact, ketoconazole has been used to treat men with metastatic prostate cancer who present with spinal cord compression.
As with LHRH agonists/antagonists, chemical castration will result in profound side effects due to very low hormone levels. Ketoconazole is no longer used as first line therapy due to the advent of more effective antifungal agents and it’s significant side effect profile.
Even lower doses of ketoconazole can lower testosterone levels when used for a prolonged period of time.
High Blood Pressure Drugs
High blood pressure or hypertension is a common condition in men. Up to 50% of men in the United States have hypertension and many of them don’t even know it. The exact pathophysiology of primary hypertension is unclear but it’s called the “silent killer” for good reason. Secondary hypertension is due to an underlying medical condition like renal artery stenosis and occurs in about 10% of cases.
The Risks of High Blood Pressure
High blood pressure increases the risk of heart attack, stroke, dementia and kidney disease. Due to it’s immense impact on men’s health, I’m going to say a few things about hypertension before we get into the medications used to treat high blood pressure that may lower testosterone.
As a urologist who specializes in men’s health, I see a lot of men who are concerned about low testosterone and it’s negative impact on health. Low testosterone can increase the risk of insulin resistance, metabolic syndrome, depression and osteoporosis. But many of these men have untreated hypertension which carries far greater risk to their health and well-being.
Normal Blood Pressure and the Deadly Risk of High Blood Pressure
Normal blood pressure is defined as a systolic blood pressure of 120 mm Hg or less and a diastolic blood pressure of 80 mm Hg or less. Consider this eye opening scientific fact. If you have a systolic blood pressure of 140 mm Hg your risk of death is DOUBLED compared to men who have a normal systolic blood pressure of 120 mm Hg. Research suggests that the greater the blood pressure elevation, the greater the risk of death from cardiovascular events such as heart attack and stroke. High blood pressure also increases the risk of dementia and end stage kidney disease substantially.
Hypertension is Asymptomatic so it must be Measured
Hypertension is generally not associated with any symptoms so unless you properly measure your blood pressure you will not know if you have hypertension or not. Best methods for measuring blood pressure accurately are straight forward but rarely done correctly at the doctor’s office. How to properly assess high blood pressure is beyond the scope of this article but at my practice we try to obtain a legitimate assessment of every patient’s blood pressure on a regular basis.
High Blood Pressure and Men’s Health
Why do I care about high blood pressure as a men’s health specialist? Because your risk of serious health issues and death are far greater due to your elevated blood pressure compared to your low testosterone. Furthermore, testosterone therapy can worsen hypertension in some men exacerbating the ominous risks of elevated blood pressure. Making matters worse is the fact that high blood pressure causes erectile dysfunction, a condition no man wants to deal with.
Treatment of High Blood Pressure
At my practice, we refer men to internal medicine or cardiology for aggressive management of hypertension. Fortunately, lifestyle modifications can have a positive effect on hypertension but medications are often required to truly minimize risk.
There are several classes of prescription medications used to treat high blood pressure. First line therapy usually includes one of four classes of medication including ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers and thiazide diuretics. In resistant cases, beta blockers, alpha blockers and other diuretics may be needed.
Spironolactone
Spironolactone is medication used to treat high blood pressure and heart failure. It is a mineralocorticoid receptor antagonist. Mineralocorticoids like aldosterone cause sodium and water retention which increases blood pressure. Aldosterone is essential for life but too much of it can cause problems.
Blocking the effect of aldosterone with spironolactone causes sodium and water loss Idiuresis) which can lower blood pressure and treat the fluid overload associated with heart failure.
Spironolactone interferes with the steroidogenic enzymes involved in testosterone synthesis. It also may increase SHBG levels thereby reducing bioavailable testosterone levels. It also works as a non-specific androgen receptor antagonist or antiandrogen. As you can see, spironolactone is a good example of a prescription medication that can negatively impact testosterone physiology through several mechanisms. Interestingly, spironolactone is used to treat polycystic ovary syndrome in women.
Beta Blockers
Beta blockers are another class of hypertension medications used to treat high blood pressure and heart disease. Several beta blockers have been shown in small studies to lower testosterone levels. They most likely cause this reduction in testosterone by affecting pituitary-hypothalamic signaling. Beta blockers can also cause erectile dysfunction by other mechanisms.
Thiazide Diuretics
Thiazide diuretics are often used as first line therapy in men with hypertension. These drugs work by blocking sodium and water absorption in the distal tubules of the kidney. Research suggests thiazide diuretics may decrease bioavailable testosterone levels.
Antidepressants and SSRIs
Depression can have it’s own deleterious effects on sexual function and libido. Low testosterone can potentially lead to depression and dysphoria. Treatment of low testosterone can have a favorable impact on mood. While some cases of depression may respond to testosterone replacement therapy, many emphatically do not and will still require antidepressants.
SSRI Mechanism of Action
Selective serotonin reuptake inhibitors or SSRIs are a class of drugs used to treat depression and mood disorders. As their name implies, SSRIs inhibit the reuptake of serotonin which makes more serotonin available to the neurons. This generally improves the chemical imbalance responsible for some types of mood disorders.

SSRI Side Effects
SSRIs are quite effective at treating depression and are often first line therapy for men suffering from mood disorders. However, they do cause quite a few side effects including sexual dysfunction. Men taking antidepressants can experience low libido, erectile dysfunction and difficulty reaching an orgasm. These sexual side effects can be devastating to men already dealing with a depressive disorder. Alternative medications are sometimes required to mitigate side effects.
Sexual Side Effects of SSRIs Explained
SSRIs cause sexual dysfunction by a variety of mechanisms. One such mechanism is via low testosterone. SSRIs reduce testosterone synthesis by inhibiting CYP-17 steroidogenic enzymes. SSRIs also may stimulate aromatase activity which converts more testosterone into estradiol. It is also possible that they exert a central effect in the brain to decrease LH secretion.
Increased Prolactin due to SSRIs
Complicating matters further is the fact that SSRIs can increase prolactin levels. Prolactin is a hormone secreted by the pituitary gland. Excessive levels of prolactin can inhibit the secretion of GnRH and thereby cause low testosterone by suppressing LH secretion by the pituitary gland.
Selective serotonin reuptake inhibitors are another example of medications that lower testosterone via more than one mechanism.
Antipsychotic Medications
Schizophrenia and other related mental health conditions affect less than 1% of the U.S. population but these conditions cause significant distress to patients and caretakers alike. Medications used to treat schizophrenia are called antipsychotics and are known to cause sexual side effects.
While antipsychotic medications may have central nervous system effects that impair sexual performance they can also increase prolactin levels. Increased prolactin levels will lead to low testosterone levels in some men taking these drugs.
As with any medication associated with a low testosterone state, men on antipsychotics should be monitored for low T symptoms and sexual side effects.
Chemotherapy and Cancer Survivors
Despite aggressive early detection strategies for some cancers, about two million US citizens will be diagnosed with cancer annually. It is one of the most devastating diagnoses one can receive from their physician.
Cancer can be treated with surgery, radiation and chemotherapy. Some cancers require a combination of these treatments.

Cancer treatment can cause low testosterone depending on the therapies deployed by your oncologist.
Cancer Surgery
Surgery to remove the testicle is necessary for testicular cancer and is used in some cases of prostate cancer.
Prostate Cancer and Testicle Removal
Bilateral orchiectomy is a procedure sometimes done to treat locally advanced or metastatic prostate cancer. Removal of both testicles will obviously lead to castrate testosterone levels. As discussed, drugs like LHRH agonists and antagonists can be used in lieu of surgical orchiectomy. Some men prefer chemical castration due to the psychological burden associated with surgical castration.
Castrate testosterone levels will lead to profound symptoms of hypogonadism. Some of these symptoms can be mitigated with lifestyle modifications such as a healthy diet and exercise. Prescriptions medications can also be used to mitigate some of the side effects of castration.
Surgery for Testicular Cancer
Unilateral orchiectomy is a procedure to remove one testicle. This is typically done for testicular cancer which is almost always a unilateral disease. Bilateral testicular cancer requiring removal of both testicles is quite rare although I just saw a young police officer who required it.
Testicle Removal for Benign Disease
Orchiectomy is also done for benign diseases such as chronic infection, abscess and other pathology. Some men are born with one testicle while others may have an undescended testicle that requires surgical removal due to an elevated risk of cancer.
Unilateral orchiectomy removes half of the testosterone producing tissue in the body. Sometimes, the remaining testicle can increase production and make up for the loss. However, some men will definitely see a clinically significant decrease in testosterone levels warranting therapy.
Radiation
Radiation therapy is often used to treat a variety of malignancies including pelvic cancers. While the testicles can often be shielded during treatment, they can sometimes be damaged by radiation therapy to the pelvis or upper thighs.
Radiation damage to the testicle can destroy Leydig cells in the interstitial tissues leading to reduced testosterone production.
Chemotherapy
A multitude of drug classes are utilized as chemotherapy to treat cancer. We have already discussed the LHRH agonists and antagonists which are used to treat advanced prostate cancer. These prescription medications lower testosterone to castrate levels by shutting down LH production by the pituitary gland.
Cytotoxic Drugs
Classic chemotherapeutic drugs are cytotoxic in nature. Through a variety of mechanisms they damage DNA and other cell pathways that lead to cell death. Typically, cytotoxic chemotherapy drugs are designed to work on rapidly dividing cells. Cancer is essentially a group of cells that divide at an abnormal rate leading to tumor growth.
By targeting these rapidly dividing cancer cells, cytotoxic chemotherapy can selectively target cancer cells. Unfortunately some normal cells in the body will be affected by cytotoxic chemotherapy, especially cells that divide relatively fast. This may include cells that line the GI tract for example which accounts for the nausea and vomiting associated with chemotherapy.
Cytotoxic Chemotherapy Damages the Testicle
Some tissues in the body are particularly sensitive to cytotoxic molecules, the testicle being one of them. Cytotoxic chemotherapy often damages the testicle causing both infertility and low testosterone. Sometimes the testicle can recuperate function once chemotherapy has been completed but in some cases permanent damage can be done.
Targeted Immunotherapy
Targeted immunotherapy drugs are relatively new compared to cytotoxic chemotherapy. As their name implies, these drugs target specific pathways in particular cancers by modulating immune function. Their effects on testosterone levels are a bit unclear although at least one study in melanoma patients found a reduction in testosterone levels in men on immunotherapy.
Opioid Pain Medications
Opioids are a group of analgesic medications used to treat acute and chronic pain. Opioids are classified according to their mode of synthesis and include alkaloids, semi-synthetic and synthetic molecules. Opioid pharmacology started with the discovery and isolation of morphine in the early 1800’s.
Morphine and it’s derivatives are still used today but newer compounds such as oxycodone and hydrocodone are also popular analgesics in common use. Opioids bind to opioid receptors in the central nervous system to exert their analgesic effects although opioid receptors are also found in peripheral tissues.
The Opioid Crisis
Up to 12% of the population suffers from chronic pain. Despite the “opioid crisis” a lot of prescriptions for opioids are still being written. Increased awareness has led to more careful use by physicians and they do a better job monitoring patients for tolerance and dependence. Alternative pain management strategies are also more widely understood and employed today.
Opioid Side Effects
Opioid drugs can cause serious adverse effects including depression, impaired bowel motility and urinary retention. Excessive levels of opioids can lead to respiratory depression and death if not reversed using Naloxone. Opioids can also lead to dependence and addiction. Chronic pain is not fun but neither is dependence to opioids.
Short versus Long Acting Opioids
Opioid drugs can be short or long acting opioids. Short acting opioids would be used to treat acute pain such as following a surgery or injury while long acting opioids are used to treat more chronic pain syndromes.
Opioid Induced Low Testosterone
Opioid pain medications are well known causes of low testosterone or hypogonadism. They exert this testosterone lowering effect by inhibition of the hypothalamic-pituitary axis. Lowering of LH levels decreases testosterone synthesis in the testicle. Some opioids given chronically may also increase sex hormone binding globulin levels which reduces bioavailable testosterone. While all opioids have the potential to cause low testosterone levels, short acting opioids are less likely compared to long acting opioids.
Low testosterone levels in these men will lead to sexual dysfunction, fatigue, insomnia and other symptoms of hypogonadism. Hypogonadal men are at risk for osteoporosis, depression and insulin resistance. Testosterone deficiency also leads to hyperalgesia making it even more difficult to manage the patient’s pain.
Treatment of Opioid Induced Low T
Treatment options for opioid induced low T include alternative medications, symptomatic treatment as well as testosterone replacement therapy. Testosterone replacement therapy has been well studied in chronic opioid users and clearly has many benefits.
Benefits of testosterone in these men include improved sexual function, mood, energy, sleep and pain control. Testosterone also reduces the risk of osteoporosis and type 2 diabetes mellitus. By correcting hypogonadism these men become more sensitive to pain medication so lower doses of opioids may be required.
Opioid induced testosterone deficiency is quite common so any patient on long acting opioids should be questioned about the signs and symptoms of testosterone deficiency. If symptoms are present an appropriate diagnostic work-up should take place by urology or endocrinology.
High Cholesterol and Statins
Statins are the work horse of lipid lowering therapy in the United States and we have to spend some legitimate time discussing them as they relate to low testosterone and men’s health in general.
Cardiovascular Disease is the #1 Killer of Men
Cardiovascular disease is the number one killer of men. Men are ten times more likely to die from a cardiovascular event than cancer. Think about that for a minute. If you could only choose one potential disease to avoid, it would hands down be cardiovascular disease if you wanted to live as long as possible.
Risk Factors for CVD
The three main risk factors for cardiovascular disease include smoking, abnormal blood cholesterol and high blood pressure. Other factors such as obesity and insulin resistance also play important roles. The link between elevated blood cholesterol and cardiovascular disease is firmly grounded in large scientific studies. Let me be clear, elevated LDL cholesterol is CAUSATIVE, not just associated with an increased risk of heart attack and stroke.
LDL-Cholesterol and Lipidology
We are not going to take a deep dive into lipidology here because the topic is vast. So vast in fact, that lipidology is it’s own sub-specialty among cardiologists. The bottom line is that LDL cholesterol gets into the arterial wall and causes atherosclerotic plaque. When these plaques become unstable a thrombosis occurs and the artery is occluded. This causes ischemia to the heart muscle resulting in a heart attack. If the area of ischemia is large enough, death may be the result. The presenting symptom of a first heart attack is sudden death in almost half of men.
CVD Often Presents with Death
Think about that presenting symptom for a minute. Almost half of men who have a heart attack will not present with chest pain or shortness of breath and wind up in a cardiac intervention lab for a stent. They simply die on the spot. Another concerning statistic regarding heart attacks is that 25% of men will have one before the age of 55.

All men should be concerned about cardiovascular disease because it IS the #1 disease that kills us and it’s not just a disease of older men. Since elevated LDL cholesterol (LDL-c) causes atherosclerosis we need to be very concerned about our lipid profiles. Two out of five men in the United States have elevated blood cholesterol.
Again, lipid testing is complicated and it goes far deeper than the routine lipid panel most physicians check but we aren’t here to get into those weeds. Discussing LDL-c is good enough for the purposes of our discussion on statins and low testosterone.
There are several classes of drugs used to treat high cholesterol but statins are usually first line therapy. Statins are very effective at lowering blood cholesterol levels, in particular LDL-c which is the main culprit in cardiovascular disease.
Statins and Testosterone Levels
Cholesterol is the precursor of all sex hormones including testosterone. Cholesterol is such an important molecule that all cells in the body can make it. Statin drugs inhibit an enzyme called HMG CoA reductase, the rate limiting step in cholesterol biosynthesis. As you will recall, the Leydig cells of the testicle can get cholesterol by making it themselves or by extracting it from circulating lipoproteins like LDL-c.
Cholesterol Metabolism and Low Testosterone
Statins shut down cholesterol biosynthesis in the Leydig cells but theoretically this shouldn’t matter since cholesterol is still present in circulating lipoproteins. However, research suggests that men on statin therapy have lower testosterone levels. Now the reduction of testosterone in one meta-analysis was 4%, not exactly a staggering reduction.
Some researchers have suggested that the testosterone lowering effect of statins may reduce atherogenesis and perhaps may contribute to the adverse effect of type II diabetes seen in men using statins.
Although the reduction in testosterone levels is small, is it enough to cause symptoms of low testosterone? Unfortunately we do not have a clear answer to this question. Normal testosterone levels are wide ranging and some men may experience a more significant lowering of testosterone when high dose statins are employed.
Non-Prescription Medications that Lower Testosterone
While numerous prescription medications can lower testosterone levels, there are several non-prescription drugs which can also induce hypogonadism.
Cimetidine
Cimetidine is an H2 receptor antagonist used to treat acid reflux and ulcer disease. It is now available without a prescription. Cimetidine likely impairs testosterone production by inhibiting one of the steroidogenic enzymes in the testosterone synthesis pathway. Like most of the drugs we are discussing, the low testosterone effect is reversible upon drug cessation.
A newer class of drugs called proton pump inhibitors do not adversely effect testosterone levels and tend to work better at reducing the acid in the intestinal tract.
Alcohol
Yes, alcohol is a drug and it can lower testosterone. I see patients who consume alcohol in varying degrees ranging from social drinking (1-2 drinks per week) to heavy consumption (2 or more drinks daily).
Alcohol and Health
Let me be clear on this next point as a doctor who specializes in men’s health. There is no amount of alcohol that is healthy. Alcohol may be the quintessential social lubricant but it has nothing but deleterious effects on health.
In both men and women, alcohol leads to liver disease and hypertension. Alcohol consumption also increases the risk of cardiovascular disease, the number one killer of both men and women.
Alcohol is pure sugar making it terrible for insulin resistance, fatty liver disease and metabolic syndrome.
Alcohol and Sexual Dysfunction
Given alcohol’s adverse effect on vascular and metabolic health, it is no surprise that it contributes to erectile dysfunction in men. To make matters even worse in the sexual function department, alcohol lowers testosterone levels.
Alcohol and Lower Testosterone
Alcohol adversely effects testosterone physiology at multiple levels. It impairs hypothalamic and pituitary function which lowers LH levels. Alcohol also directly impairs Leydig cell function thereby reducing testosterone synthesis directly.
Alcohol and Increased Estrogen
The long term effects of alcohol include mental health conditions such as anxiety. Another side effect of alcohol is that it may potentially lead to higher estrogen levels. Higher estrogen levels in the face of low T is not a good thing on many levels. An adverse effect of higher estrogen levels is abnormal fat distribution in men as well as gynecomastia.
When it comes to sex drive, erectile function and testosterone, alcohol does nothing but wreak havoc. When patients come to me with lower testosterone levels, I always ask about alcohol consumption and discuss the importance of reduced use and preferably, total cessation.
Marijuana and THC Products
The studies on marijuana and THC’s effect on testosterone levels are conflicting. Some data suggests that testosterone levels are lowered while others actually demonstrate an increase in serum testosterone in marijuana users.
My Clinical Experience with Marijuana and Low Testosterone
In my clinical experience, marijuana does tend to lower testosterone especially in heavy users. The occasional marijuana cigarette may transiently lower testosterone but I’m far more concerned about the chronic user. Chronic marijuana use causes other issues beyond low testosterone and sexual dysfunction in men.
THC Edibles and Testosterone Levels
One study demonstrated that oral THC use caused testicular atrophy and lower testosterone levels in animals.
Illicit Drugs and Hypogonadism
Illicit drugs include a variety of molecular compounds including narcotics, stimulants like cocaine and psychedelics. Narcotics would fall under the category of opioid medications and lower testosterone by the same mechanisms. Understanding how other illegal drugs affect testosterone levels is difficult to study for obvious reasons. If you are using illicit drugs you probably have bigger fish to fry than worrying about how these drugs impact your testosterone levels.
Illicit Drugs and Sexual Performance
Regardless of testosterone levels, recreational drugs have a negative impact on sexual function and overall health. This is not even debatable.
Anabolic Steroids
Anabolic steroids comprise testosterone and its synthetic derivatives. These compounds have been used for decades by professional athletes to enhance performance and build muscle mass. Anabolic steroid use has increased among amateur athletes as well. Studies have suggested that anabolic steroid use is the number one cause of low testosterone in young men.
Anabolic Steroids and the Pituitary Gland
All anabolic steroids drastically suppress the hypothalamic-pituitary axis which results in markedly low LH and FSH levels. This leads to decreased spermatogenesis and infertility along with testicular atrophy. Leydig cell function ceases along with endogenous testosterone production.
Anabolic Steroids taken with Testosterone
As long as men are taking testosterone along with their other anabolic steroids they will not experience the symptoms of hypogonadism. In other words, the decreased testosterone levels in the testicle are not experienced since systemic testosterone levels are maintained by the synthetic testosterone.
Stopping Anabolic Steroids
The problem arises when they stop anabolic steroids. Some men who abuse anabolic steroids for a few short time periods may recover their endogenous testicular function in 6-12 months. However, more chronic use of anabolic steroids can lead to permanent hypogonadism in these men. Lower hormone levels of LH and FSH persist leading to permanent subfertility and low testosterone.
Treatment of Anabolic Steroid Induced Hypogonadism
Anabolic steroid induced hypogonadism can be difficult to treat. Some men may respond to LH and FSH administration but testicular function does not always return. In men with persist testicular dysfunction, testosterone replacement therapy will be needed to restore normal hormone levels. Infertility may also persist and necessitate assisted reproductive technology to conceive a child although this is not always possible.
Clinical Implications
So we have now covered testosterone physiology with quite a bit of detail so we can understand how prescription medications and other drugs impact testosterone levels in the human body. We have discussed a laundry list of molecules that may lower testosterone to varying degrees.
Now we need to get to the guts of the conversation. How do these particular drugs effect patients on the individual level? How much do they lower testosterone in patients and will they develop symptoms of low testosterone? What is the approach physicians should use to investigate the possibility of low testosterone in men taking these medications? If low testosterone is diagnosed, what is the best course of action?
Recognition of Low T Symptoms
If you are on a drug that may lower testosterone, the initial question to ask is, are you having symptoms of low testosterone? Symptoms of low testosterone include low libido, erectile dysfunction, fatigue, lack of motivation, insomnia, depressed mood, increased belly fat, difficulty building muscle mass and getting through work-outs.
Physical Signs of Low Testosterone
The physical signs of low testosterone may include atrophic testicles, gynecomastia, reduced body hair and increased adipose tissue around the midsection.
Next Steps for Men with Symptoms or Signs of Low Testosterone
If you have symptoms or physical signs of low testosterone then it’s time to get evaluated, preferably by a urologist. Men with signs of symptoms of low testosterone warrant a medical evaluation, period.
Basic Lab Testing for Men Suspected of Having Low Testosterone
At the very least, men experiencing symptoms or signs of low T should have at least two morning (between 8-11 AM) total testosterone levels measured at a reputable lab using validated testosterone assays. At our practice, we prefer to measure both free and total testosterone levels during our assessment of men with low T symptoms.
Diagnostic Criteria for Making the Diagnosis of Low Testosterone
According to the guidelines from the American Urologic Association, the laboratory diagnosis of low T is made when men have two total testosterone levels below 300 mg/dL. Of course, not all men will follow these strict guidelines. In fact, European guidelines use 350 ng/dL as the cutoff for normal. Furthermore, some men with low normal testosterone levels may still benefit from testosterone replacement therapy.
Additional Testing Once the Diagnosis of Low T is Made
Once the laboratory diagnosis of low testosterone is confirmed, two things need to happen. Your doctor should do additional testing to look for underlying causes of low testosterone such as pituitary or thyroid disease. Secondly, a comprehensive medical evaluation should also take place to make sure no other medical issues are contributing to the patient’s symptoms. This will also ensure that no medical contraindications to testosterone treatment are present as well as identify certain medical issues that my be due to low testosterone such as insulin resistance.
Recognition of Drugs that Lower Testosterone
If you are diagnosed with low testosterone, your physician should take a hard look at your medications to see if any of them could be lowering testosterone levels. As you can see from this lengthy article, there is a laundry list of drugs that can lead to a low testosterone state.
Now, we know that not all physicians are created equal, so this may be something easily missed by a doctor. Be your own health advocate after reading this article and let your physician know that you are taking a medication that has been linked to lower testosterone levels.
Treatment Options for Low T Patients on Drugs that May Lower Testosterone
So now we are getting to the heart of the conversation. You have been properly diagnosed with low testosterone but happen to be using a drug or drugs that have been reported to lower testosterone levels. Is the drug the cause of your low testosterone or not? That is the big question this article needs to answer.
Like many things in medicine, there is no easy answer here. Good medicine is an art based on science. So, how does the astute clinician approach this situation?
Normal Testosterone Levels are Wide Ranging
We have to keep in mind that normal testosterone levels are wide ranging. Normal total testosterone levels range from 300-1,200 ng/dL. That is an enormous reference range and most people have no idea where they started from. Routine assessment of testosterone levels in healthy men is not something we measure. Testosterone levels are not tested until men are having symptoms so we almost never understand someone’s baseline.
Drugs that Lower Testosterone have Wide Ranging Effects
Some drugs lower testosterone drastically, even to castrate levels. As you recall, LHRH agonists and antagonists are used to chemically castrate men with advanced prostate cancer. We know these drugs have a very consistent and dominant effect in ALL men. Anabolic steroids lower testosterone in ALL men. There is no question these drugs are the culprit.
But it’s not so straight forward with other drugs that lower testosterone. Many of the prescription medications we discussed don’t seem to lower testosterone all that much. For example, a statin tends to lower testosterone levels by about 4%. If your testosterone was 400 ng/dL before starting a statin that would mean a decline of 16 ng/dL bringing your total testosterone to a level of 386 ng/dL. A total testosterone of 386 ng/dL is still within the normal range according to the American Urologic Association.
Most men are simply not going to notice a testosterone decrease of 4%.
Patients are Not Populations
We also must recognize that not all patients follow population based findings. Studies always have outliers. So, it is certainly feasible that a statin may lower testosterone levels more than 4% in some men. The same applies to other drugs that may have quite varying effects on lowering testosterone levels in the individual patient.
Perform the Experiment
If a patient is diagnosed with low testosterone and is using a drug known to lower testosterone levels, we can always do the “experiment”. The “experiment” means stopping the drug to see if testosterone levels increase and low T symptoms resolve.
This is the same simple experiment we do in medicine all the time when patients experience a side effect after starting a drug. Not all side effects are reported in the scientific literature. So, if someone is having a side effect not previously reported, it’s easy enough to stop the drug and see if the side effects resolves.
The Experiment Must be Safe
Now, if we decide to perform this drug holiday experiment we must do it in a safe manner. Not all drugs can be safely stopped so do NOT try this without medical supervision. Some drugs simply cannot be stopped safely, such as a blood pressure medication in a patient with heart failure. We also wouldn’t want to stop an antidepressant drug in someone with major depression and a history of suicide attempts.
Even if a drug can be stopped in a safe manner, sometimes they have to be weaned. A cold turkey stop is not always feasible.
Alternative Medications
If it’s not safe to stop a drug we can always look at alternative medications instead. If someone is on a blood pressure medication that lowers testosterone levels perhaps we can switch them to a different antihypertensive drug that is NOT associated with a testosterone lowering effect. If testosterone levels improve, we have our answer without putting their health at risk.
Of course, stopping a medication or switching to an alternative medication is not always straight forward. It requires careful medical supervision.
Timing of Testosterone Recovery
If a potential testosterone lowering drug is stopped, we have to consider the timing of testosterone recovery to carry out the experiment correctly. Depending on the mechanism by which the drug is lowering testosterone levels, it could take the body weeks or even months to recuperate.
So, if you stop a potential low T drug offender, plan on following your testosterone levels for months before you can make any experimental conclusions. Depending on the drug, I usually tell my patients it will take 6-12 months to see their drug holiday experiment to its conclusion.
Should we Always Stop Drugs that may Lower Testosterone?
This is where the art of medicine comes in to play. When I am faced with this situation the plan must be highly individualized. I certainly review the scientific literature on the drug with my patient. We then look at how low their testosterone levels are. Does the science suggest a clinically significant lowering of testosterone levels or not?
I also will take into account my clinical experience with the same drug in other patients. Of course, patient preferences also sway decision making. Using this individualized approach with shared decision making between patient and physician it’s generally pretty easy to come up with a logical plan.
Sometimes men will decide to take a drug holiday and follow testosterone levels for 6-12 months. Other men will decide not to do the experiment if there is a low likelihood of seeing testosterone levels recover fully.
What if the Experiment Fails?
If you stop the potential offending drug and testosterone levels do not improve significantly then we would consider testosterone replacement therapy. In my experience, men on drugs that lower testosterone are more likely to have idiopathic hypogonadism than drug induced hypogonadism. When the experiment fails, we simply treat them like any other patient with low testosterone.
What if the Experiment is NOT Performed?
After a thorough discussion, some men will decide not to stop the potentially offending drug. They decide not to embark upon the drug holiday experiment. We treat these men like any other patient with low testosterone.
The Drug Holiday That Never Fails
Never say never in medicine, I certainly subscribe to that. However, I always tell men with low testosterone that the best course of action is to stop alcohol, THC and illicit drugs if they are being ingested.
This experiment never fails because men will always feel better and improve their health even if testosterone levels do not improve. If low T symptoms and low testosterone levels persist, I will certainly treat them like any other patient with testosterone deficiency. However, the results of testosterone replacement therapy are always superior when these drugs are stopped or greatly reduced.
Anabolic steroids also need to be stopped immediately, especially in men wishing to father children.
Concluding Statement
Low testosterone is a common condition in men. Many prescription medications and other drugs can lower testosterone levels or create a state of low testosterone.
If you have symptoms of low testosterone, see a urologist. A urologist will perform a diagnostic work-up. If the diagnosis of low testosterone is confirmed with lab testing, medications that may lower testosterone should be examined.
If the patient is on a drug that may lower testosterone, a thoughtful conversation should ensue to assess the relevance of a drug holiday experiment. If the experiment fails or the patient decides to forego the experiment, testosterone replacement therapy should be considered after a careful review of risks.
