In this article, we will discuss testosterone replacement therapy in detail. We will address the indications for testosterone therapy along with the associated risks of treatment. In particular, we will address the mental health benefits and behavioral side effects associated with injections of testosterone. If you don’t need or want a thorough refresher on testosterone deficiency you can skip to the section titled “Mental Health Consequences of TRT and Low Testosterone” for the specifics on that subject.
What is Low Testosterone?
Low testosterone is a medical condition that develops when testosterone levels drop below normal (total testosterone less than 300 ng/dL). These low testosterone levels lead to bothersome symptoms and metabolic derangements. Low testosterone is also called hypogonadism, testosterone deficiency syndrome, androgen deficiency of the aging male or just “low T”. Low testosterone can be caused by underlying medical conditions, prescription medications and testicular failure. Many cases of low testosterone are idiopathic, meaning no definitive cause can be identified.
What are the Symptoms and Signs of Low Testosterone?
When testosterone levels fall below the normal range (total testosterone less than 300 ng/dL), men can experience a variety of manifestations including sexual symptoms such as low libido, erectile dysfunction and delayed ejaculation. Other symptoms of male hypogonadism may include fatigue, irritability, depressed mood, insomnia, impaired cognitive functions, mood swings and lack of motivation. Physical indicators of low testosterone may include increased body fat, difficulty building muscle mass, impaired recovery from work-outs and reduced exercise endurance.

Men with low testosterone levels can also present with physical signs of hypogonadism along with subjective symptomatology. Physical signs of hypogonadism may include atrophic testicles (reduced testicular size), lack of secondary sex characteristics, reduced body and facial hair, breast enlargement and alterations in body composition including increased belly fat and/or lack of muscle mass.
Health Consequences of Hypogonadism
A testosterone decline can certainly cause a multitude of low T symptoms and physical signs in men. It can also lead to adverse health consequences when left untreated. Low testosterone levels increase the risk of osteoporosis (low bone density), depression, loss of muscle mass/strength, insulin resistance and metabolic syndrome. Men with low T often struggle with weight loss leading to an increased risk of obesity.
Metabolic syndrome was originally called syndrome X and is a cluster of conditions associated with metabolic dysfunction. Metabolic syndrome includes hypertension, insulin resistance, increased truncal obesity, elevated triglycerides and low HDL-cholesterol. Metabolic syndrome and it’s associated hyperinsulinemia increases the risk of cardiovascular disease, cancer and neurodegenerative diseases such as Alzheimer’s disease.
Some studies have suggested that low testosterone levels are associated with an increased risk of aggressive prostate cancer and heart disease although this is somewhat controversial.
Testosterone Physiology
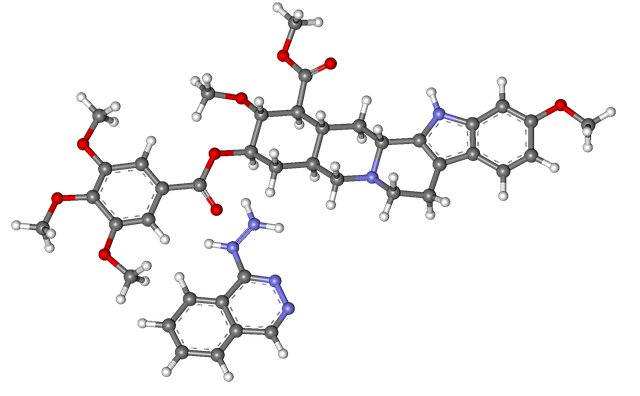
Testosterone is the quintessential male sex hormone or androgen. Understanding it’s physiology is important when trying to master the complexities of male hypogonadism. Testosterone is a powerful anabolic hormone along with growth hormone and insulin-like growth factor (IGF). Anabolic hormones promote growth and proliferation of certain tissues. Testosterone is very anabolic in the muscle by promoting muscle protein synthesis. This is the reason testosterone and many of it’s derivatives (oxandrolone and trenbolone) are abused by athletes and bodybuilders.
Testosterone production takes place in the Leydig cells of the testicles. The testosterone molecule itself is derived from cholesterol. Complex steroidogenic enzymes in the testicle are required to convert cholesterol into the active testosterone molecule. Cholesterol can be synthesized by the Leydig cell or obtained from circulating lipoproteins when additional testosterone production is needed. Lipoproteins are particles such as LDL (low density lipoprotein) and HDL (high density lipoprotein) which transport cholesterol and phospholipids in the blood.
The Leydig cells of the testicle are under the control of luteinizing hormone (LH), a molecule secreted by the pituitary gland. LH secretion stimulates testosterone synthesis by the Leydig cell. Follicle stimulating hormone (FSH) is also secreted by the pituitary gland and acts on the Sertoli cells of the testicle to promote normal sperm production. Sertoli cells also act in a paracrine fashion on the Leydig cells, promoting normal testosterone biosynthesis.
The pituitary gland is the master gland of the human body and sits at the base of the brain. The pituitary gland controls the testicle through LH and FSH secretion but also presides over other glandular structures including the thyroid and adrenal glands. The pituitary gland is modulated by the hypothalamus so both structures are essential for normal sex hormone production. The hypothalamus secretes a hormone called luteinizing hormone releasing hormone (LHRH) in a pulsatile manner which directs the pituitary to secrete LH. LHRH is also referred to as gonadotropin releasing hormone (GnRH).
Drugs or medical conditions that have significant effects on the hypothalamus or pituitary can impact testicular function.

Sex Hormone Binding Globulin (SHBG) and Bioavailable Testosterone
Testosterone made by the Leydig cells enters the blood stream where most of it is bound by circulating blood proteins. The two predominant testosterone binding proteins are sex hormone binding globulin (SHBG) and albumin. Orosomucoid and corticosteroid binding globulin (CBG) also bind to testosterone but the clinical significance of these proteins is poorly understood.
The sex hormone binding globulin (SHBG)-testosterone bond is so tight that testosterone is trapped in the blood stream by this protein. To the contrary, the albumin-testosterone bond is weak so that albumin bound testosterone can easily enter tissues to exert it’s powerful hormonal effects.
SHBG levels are heavily impacted by genetics as well as three other hormones: estradiol, thyroid hormone and insulin. High SHBG levels can lower free and bioavailable testosterone (explained below). Disorders of the thyroid gland and insulin resistance can alter SHBG levels and put men at risk for hypogonadism.
A small fraction (1-2%) of testosterone is free or unbound in the serum. The free testosterone along with albumin bound testosterone is called bioavailable testosterone. Bioavailable testosterone is what matters physiologically since it has the capacity to leave the blood stream and enter tissues. If most of the testosterone in the blood is bound to SHBG, a low testosterone state is created despite normal total testosterone values (greater than 300 ng/dL).
Free testosterone and bioavailable testosterone can be measured on a laboratory test. Clinical assays of bioavailable testosterone can be inconsistent. Validated free testosterone assays are available and may correlate with bioavailable testosterone levels better than total testosterone.
Men with normal total testosterone levels and symptoms of hypogonadism should have SHBG and free testosterone levels measured. Evidence of low free testosterone levels in the face of hypogonadal signs or symptoms may warrant a trial of testosterone replacement therapy.
The effects of testosterone are modulated by the androgen receptor (AR) which is located in the cytoplasm of the cell. Testosterone must bind the AR receptor and this testosterone-AR complex can then enter the nucleus of the cell and alter the transcription of genes. These genes will produce messenger RNA (mRNA) that will eventually get translated into proteins by the ribosomes. Proteins include receptors and enzymes that can alter cellular and organ function.
Alterations in the androgen receptor can disrupt normal testosterone signaling. Androgen receptor differences exist between individuals but clinical testing to assess androgen receptor sensitivity is not available. But, if someone has insensitive androgen receptors they probably require higher serum testosterone levels to function normally. Contrarily, men with very sensitive androgen receptors need very little testosterone to be physiologically intact.
These androgen receptor differences can sometimes impact decision making for men with hypogonadal symptomatology.
Estradiol and Dihydrotestosterone (DHT)
A small fraction of testosterone is converted into estradiol by an enzyme called aromatase. Estradiol is the predominant estrogen in men. Aromatase is located primarily in the adipose or fat tissue. Estradiol is an important sex hormone in both men and women. Estrogens in men are essential for normal erectile function and building muscle mass. They are also essential for normal brain function, bone density and cardiovascular health.
Estradiol works in a negative feedback loop on the pituitary gland and hypothalamus. When estradiol binds to estrogen receptors in the pituitary gland, LH secretion and testosterone biosynthesis are reduced leading to a decline in blood testosterone levels. Estrogen levels are therefore essential for modulating the amount of circulating testosterone in the body.
Excess estrogen levels in men on testosterone therapy can be problematic and may require treatment with an aromatase inhibitor. Mild increases in estrogen levels are generally considered beneficial as long as enough testosterone is present. The testosterone to estradiol ratio should be at least 10:1 for normal sex hormone physiology. Using an aromatase inhibitor for mild elevations of estradiol when the ratio of testosterone to estradiol is greater than 10:1 should be avoided.
A small amount of testosterone is also converted into dihydrotestosterone (DHT) by the enzyme 5-alpha reductase. DHT is a potent androgen molecule that stimulates prostate growth and also works on the hair follicle. It is a very potent androgen in early life involved in the development of normal male characteristics. Male children born with a deficiency of the 5-alpha reductase enzyme will have female genitalia.
An increase in DHT levels in adults can increase the risk of male pattern baldness and benign prostatic hyperplasia (BPH). BPH is a benign enlargement of the prostate gland that leads to lower urinary tract symptoms such as frequency and urgency of urination. DHT metabolites are potent neuroactive steroids and likely play a role in sexual function and mood.
Men with prostate enlargement and hair loss are sometimes treated with the 5-alpha reductase inhibitors finasteride and dutasteride. These drugs will increase testosterone levels while decreasing DHT levels by blocking the conversion of testosterone into DHT by the 5-alpha reductase enzyme. While these drugs are effective at treating BPH and hair loss, they have been associated with significant side effects including post-finasteride syndrome (PFS).
Post-finasteride syndrome symptoms include poor sexual function including erectile dysfunction and low libido along with severe depressive symptoms. Some men will continue to experience these devastating effects despite drug cessation. Men considering 5-alpha reductase inhibitors should be warned of PFS prior to starting these drugs.
Diagnosis of Low Testosterone
Men who present with low T symptoms and/or signs of hypogonadism warrant a thorough medical evaluation. This should include a complete medical history, physical examination and laboratory assessment. Men who meet the diagnostic criteria for low testosterone should be offered a trial of testosterone replacement therapy after a discussion of risks.
The diagnosis of low testosterone requires laboratory evaluation of testosterone levels in the blood. Two morning (8-11 AM) testosterone levels should be obtained. Preferably, both free and total testosterone levels should be measured. If results are equivocal, additional measurements may be warranted.
Not all testosterone assays are created equal. Poor quality assays of the sex hormones can easily misdiagnose a patient. Urologists who specialize in testosterone deficiency or andrology will be well versed in the complexities of laboratory testosterone measurement.
Other diagnostic tests such as dual x-ray absorptiometry may be used to assess bone density and muscle mass. Blood tests to assess metabolic health may also be useful since metabolic derangements can be associated with low testosterone. Measurement of pituitary and thyroid hormones is also an important part of the diagnostic process.
Normal Free & Total Testosterone Reference Range
The normal reference range for testosterone will vary between labs but generally runs between 300-1,200 ng/dL for total testosterone. Free testosterone should be between 5-25 ng/dL. These reference ranges typically encompass 95% of the population. So to be considered “low” by most guidelines you would need to have a testosterone level in the bottom 5% of the population.
Not all guidelines are in agreement. For example, the American Urologic Association uses a lower cutoff for normal testosterone of 300 ng/dL while European guidelines use 350 ng/dL. If your testosterone is 325 ng/dL you would be considered “normal” in the US but low by European standards. Complicating matters further is the fact that some men may have androgen receptor abnormalities requiring higher levels of testosterone for normal physiology to occur.
Due to androgen receptor differences and physiologic variability at the individual level, some men with low normal testosterone levels may still benefit from a trial of hormone replacement therapy. Population based guidelines are not always ideal for diagnosing and treating the individual patient.
Excluding Underlying Medical Issues
Once the diagnosis of low testosterone is made, underlying medical issues must be excluded. Certain medical conditions can cause testosterone deficiency or complicate testosterone therapy. Diagnostic testing should include biomarkers of metabolic health, lipid profiles, pituitary hormones, kidney and liver function tests, complete blood counts and thyroid hormones.
Patients will often ask for growth hormone testing which is not typically required for a patient with hypogonadism. Growth hormone deficiency is quite rare and measuring growth hormone requires sophisticated testing.
One of the most common causes of low testosterone in young men is anabolic steroid use. Anabolic steroids can lead to hypogonadism and infertility. Other medications including statins, blood pressure medications and opioids can also lower testosterone levels. A careful assessment of prior and current drug use is therefore imperative.
Underlying causes of low testosterone such as hypothyroidism, hemochromatosis, sleep disturbance and pituitary adenomas can be effectively treated so that testosterone therapy can be avoided. Up to 20% of men properly evaluated will have a correctable cause for their testosterone deficiency.
It is unacceptable for a physician to treat a patient with lifelong hormone replacement therapy when a correctable underlying issue is at play. Furthermore, underlying medical issues such as pituitary tumors and hypothyroidism can have their own deleterious health effects independent of testosterone values. An exhaustive search for medical causes of low testosterone must be performed before prescribing testosterone replacement therapy.
In addition, medical contraindications to testosterone therapy have to be dealt with before prescribing testosterone replacement therapy. These are medical issues that would increase the risks of testosterone replacement therapy or make it downright dangerous. Such medical concerns may include uncontrolled high blood pressure, high cholesterol, liver disease, blood clots, sleep apnea, prostate cancer, severe BPH, breast cancer or unstable heart disease.
Testosterone Replacement Therapy
Once an accurate diagnosis of testosterone insufficiency is made and medical contraindications have been excluded, a conversation regarding the pros & cons of therapy should ensue. No physician should prescribe testosterone without having a detailed discussion regarding the risks of therapy.
Hormone replacement therapy should not be taken lightly because it is generally a long term treatment that carries some inherent risk. In my experience, patients are often gung-ho to begin testosterone therapy until they get a fair and balanced view of the dangers of hormone replacement therapy. While expert physicians can mitigate the risks of therapy they cannot totally eliminate them.
Men must understand the effects of testosterone along with the dangers of androgen therapy before agreeing to be treated.
Testosterone therapy can lead to significant effects and benefits for men including:
- Improved libido and erectile function
- More energy
- Weight loss
- Improved mood and motivation
- Reduced irritability and anxiety
- Sleep improvement
- Enhanced exercise endurance and ability to recover from workouts
- Improved body composition and muscle mass
- Improved cognitive abilities
- Improvement in bone mineral density
- Enhanced insulin sensitivity
The potential risks of testosterone replacement therapy include:
- Hair loss
- Allergic reaction
- Acne
- Fluid retention
- High blood pressure
- Increased cholesterol
- Erythrocytosis
- Gynecomastia or breast enlargement due to high estrogen levels
- Enlarged prostate or BPH
- Blood clot requiring treatment with a blood thinner
- Worsening prostate cancer and breast cancer
- Mental health issues
- Chest pain or trouble breathing
Hormone Replacement Therapy
Hormone replacement therapy in men with low testosterone requires the administration of testosterone to correct low blood levels of the male hormone. Testosterone replacement therapy is NOT the same as taking anabolic steroids. Testosterone is a controlled substance so patients must have a prescription and discard any unused medication. Testosterone comes in a variety of FDA approved formulations including:
- Topical gels and creams
- Injectable testosterone
- Oral testosterone
- Intra-nasal testosterone
- Implantable testosterone pellets

The goal of taking testosterone under medical supervision is to restore normal testosterone levels. This will lead to significant benefits in approximately 90% of men. About 10% of men fail to respond to testosterone therapy in which case treatment should be stopped.
The Ideal Formulation for Testosterone Therapy
I will often get asked by patients which form of testosterone therapy is ideal, so here is how I field that question. All testosterone formulations, from oral testosterone to injections, are biochemically the same at the receptor level. They all yield a bioidentical testosterone molecule to your endogenous hormone.
In fact, there is really no such thing as “bioidentical” testosterone. This is a term used to fool men into buying expensive “proprietary blends” of testosterone from a compounding pharmacy. Usually the practices making such claims are online or strip mall clinics who charge men for these so called “bioidentical” hormones. Let me be clear, this is a farce. All modern day testosterone formulations are bioidentical once they get into the bloodstream.
Theoretically, all of the FDA approved formulations will work the same as long as adequate testosterone levels are achieved. This means that all testosterone formulations should treat low T symptoms once normal testosterone values are restored. Now, this is where it can get tricky. For example, topical testosterone often has very inconsistent absorption in men. Absorption can vary depending on skin temperature and moisture. Compounded testosterone creams and gels are even more inconsistent in their skin transmission. Oral testosterone absorption can be affected by certain foods and must be taken with a fatty meal.
The most consistent absorption I experience in clinical practice is with testosterone injections. Testosterone injections have 100% absorption so I can achieve very consistent blood levels of testosterone and it’s easy to titrate dosing. Short acting (once or twice weekly) testosterone shots are also dirt cheap compared to other forms of testosterone treatment. Excess testosterone levels will sometimes be seen with injections but these supraphysiologic levels can be mitigated with a simple change in dosing regimen. Again, medically prescribed testosterone is NOT the same as taking anabolic steroids.
So, from a theoretical standpoint, all FDA testosterone formulations are biochemically equivalent and should yield similar results when adequate testosterone levels are achieved. Practically speaking, short acting injections are the most effective means for delivering testosterone into the body with the lowest drop out rate and cost.
Testosterone Injections
Since I was asked to write this article on the mental health implications of injections of testosterone, we should cover this form of therapy in some more detail.
Testosterone supplementation using injectable testosterone is one of the most popular forms of TRT for a variety of reasons. Testosterone shots are cheap, easy to dose and highly effective. Testosterone treatment using injections is typically performed intramuscularly or subcutaneously.
Injectable testosterone prescribed by a urologist is not the same as taking anabolic steroids. Illegal anabolic steroids can cause blood clots, liver disease, allergic reactions and heart disease. Illegal steroids are also highly dangerous due to their poor quality, as they tend to be manufactured in illegal basement laboratories.
Intramuscular injections are performed once or twice a week using testosterone cypionate. Subcutaneous injections are typically done twice a week using testosterone enanthate. A long acting testosterone undecanoate injection (Aveed) is also available but this must be given every 10 weeks in a physician’s office. Aveed is a one size fits all option, meaning there is only one dose for all patients. Short acting injectable testosterone can be adjusted to meet individual testosterone requirements.
Testosterone cypionate is a bit cheaper than enanthate and more widely available at pharmacies but they have very similar pharmacokinetic properties. Testosterone enanthate may be more suited to the subcutaneous route of administration but it can also be used for IM injections without issue.
Short acting testosterone shots are performed in the upper outer thigh or glute muscle. Subcutaneous injections are performed with a smaller needle into the superficial belly fat below the umbilicus similar to insulin injections.
Testosterone shots carry the same possible side effects as other forms of testosterone therapy but they do have some unique properties. Testosterone cypionate injections are typically done weekly and this can lead to supraphysiologic testosterone levels 24-48 hours following an injection. These high testosterone levels can potentially increase the risk of erythrocytosis or elevated red blood cell counts. Subcutaneous testosterone enanthate injections have been shown to carry a lower risk of erythrocytosis due to lower spikes in high testosterone.
When monitoring men on testosterone cypionate, we typically look at testosterone levels towards the end of their injection cycle. The trough testosterone is a better guide to therapeutic dosing strategies and this testosterone level should not exceed the normal physiologic range. I prefer to keep the trough testosterone around 600-800 ng/dL.
Also unique to injectable testosterone is the potential risk of muscle pain at the injection site and the rare infectious complication. Some men will get a severe inflammatory response to testosterone shots that may mimic the signs and symptoms of infection. These reactions are usually due to an intolerance to the oil used to suspend testosterone and not the testosterone molecule itself. Switching to another oil based product will usually solve the problem.
Another complication unique to injectable testosterone is pulmonary micro-oil embolism. This occurs when oil based testosterone preparations are injected directly into the vascular system. The oil travels to the heart which pumps it to the lungs. The lungs do not react well to oil and this embolic event usually leads to chest pain, cough and trouble breathing.
Fortunately, most cases of pulmonary micro-oil embolism resolve within a few minutes without causing long term pulmonary compromise or the need for medical attention. In rare cases, more severe reactions requiring hospital admission have been documented, particularly with testosterone undecanoate injections.
Monitoring Men on Testosterone
Once testosterone therapy is begun, men require close monitoring and follow-up to reduce potential risks of treatment. Frequent lab draws may be needed at the outset of therapy to ensure proper dosing and rule out early complications such as erythrocytosis and excess estrogen. Once dosing is optimized and enough testosterone in the blood is confirmed, I follow patients every 3 months for the first two years.
Follow-up visits for men taking testosterone include an assessment of clinical benefits and questioning regarding potential side effects such as gynecomastia. Gynecomastia is often preceded by breast tenderness so this line of questioning is paramount in follow-up. Regular monitoring of estrogen levels, PSA and hematocrit is essential.
Annually, I perform a complete physical examination including measurement of blood pressure and performance of a digital rectal exam in men over 40. Once a year, I also perform a complete laboratory assessment of global health biomarkers including lipid profiles and metabolic health parameters.
Managing the Complications of Testosterone Therapy
Close surveillance of men on testosterone is imperative to reduce the risk of serious complications. Medical history and physical examination on a regular basis is paramount. When complications are recognized, swift management is essential to keep therapy ongoing and safe. Some circumstances may warrant drug cessation until the complication is stabilized or resolved.
Elevated Estrogen Levels
Some men on testosterone therapy will experience a marked increase in estradiol levels. When the testosterone to estradiol ratio is abnormal, high estrogens can cause side effects including fluid retention, mood swings, impaired sexual function and difficulty losing body fat. The most feared complication of excess estradiol is gynecomastia or breast enlargement.
Elevated estradiol levels are more likely to occur with testosterone injections and theoretically may contribute to the rare case of negative mental health parameters seen in men on testosterone shots. When estradiol levels are too high or the ratio of testosterone to estradiol is too low, treatment with an aromatase inhibitor may be indicated.
Acne and Hair Loss
Testosterone therapy can stimulate the sebaceous glands of the skin leading to acne. In most cases, the acne is mild and can be managed with topical skin washes such as CLn body or facial wash. More severe cases may require management by dermatology using oral antibiotics or isotretinoin therapy.
In rare cases, severe cystic acne may be resistant to medical therapy requiring cessation of testosterone therapy.
Some men who start testosterone replacement therapy will experience accelerated hair loss. This tends to occur predominantly in men who are genetically predisposed to male pattern baldness. When men are bothered by hair loss, hormone replacement therapy can be stopped or men can see dermatologists who specialize in hair loss management.
Treatment of hair loss may include topical Minoxidil, finasteride (Propecia), PRP injections and hair transplant. I am generally not a fan of finasteride due to the risk of sexual side effects and post-finasteride syndrome. Even topical finasteride will get systemically absorbed to some extent and I’ve seen a case of PFS due to topical finasteride applied to the scalp.
Erythrocytosis
Erythrocytosis can occur with all testosterone formulations but the incidence may be higher with testosterone injections. Testosterone stimulates the bone marrow to produce more red blood cells. When red blood cells get too numerous it’s called erythrocytosis.
Mild increases in red blood cell number are not problematic. In fact, more red blood cells means more oxygen carrying capacity. This increased oxygen carrying capacity of the blood can improve exercise endurance in men on testosterone.
However, if erythrocytosis gets severe enough blood viscosity can increase leading to clots, heart attack and stroke. Red blood cell count must be monitored in men on all forms of testosterone therapy. A blood test called a hematocrit is usually performed on a regular basis to monitor men for erythrocytosis.
If significant erythrocytosis develops (hematocrit > 54%), a dose reduction in testosterone can solve the problem. Alternatively, regular blood donation can normalize the hematocrit. For men who can’t donate blood, elective phlebotomy can be employed.
High Blood Pressure
Most men on testosterone replacement therapy will not see a significant increase in blood pressure. However, there are exceptions to just about every rule in medicine. A small number of men who begin hormone replacement therapy will see a significant increase in blood pressure leading to the diagnosis of hypertension.
If hypertension develops in a patient who recently started testosterone replacement therapy, a dose reduction may remedy the situation. If high blood pressure persists, men need to consider total drug cessation or treatment of the high blood pressure with anti-hypertensive drug therapy.
Dyslipidemia
The studies on testosterone and high cholesterol are mixed. Some men on testosterone replacement therapy will develop dyslipidemia, or abnormal lipoproteins. Lipoproteins transport cholesterol, triglycerides and phospholipids throughout the body. LDL particles tend to be atherogenic meaning they are more likely to get into the arterial wall and cause plaque formation. Arterial plaques are what lead to heart attack and stroke.
HDL cholesterol (HDL-c) is associated with lower cardiovascular risk and these particles may actually remove cholesterol from the arterial wall. Elevated triglycerides are associated with an increased risk of cardiovascular disease. Some studies have shown that androgen therapy increases HDL-c and lowers triglycerides suggesting that testosterone therapy is good for metabolic health.
In my experience, almost anything is possible when it comes to lipoprotein changes for men starting testosterone replacement therapy. It is important to track lipid profiles to ensure that overall cardiovascular risk is not increased by these lipoprotein fluctuations. The majority of men on testosterone therapy do not see a worsening of lipid profile.
Some studies suggest that testosterone therapy may actually lower LDL-c but this is something I have not seen clinically in my practice.
Elevated PSA
One of the most feared complications of testosterone replacement therapy is an increase in PSA. PSA stands for prostate specific antigen and is a blood test used to screen men for prostate malignancy. Prostate cancer is the most common non-cutaneous malignancy in men and the second leading cause of cancer death in men.
Early diagnosis of prostate malignancy is very feasible with aggressive screening protocols. Men considering testosterone replacement therapy must be screened for prostate cancer using PSA and digital rectal examination (DRE). Testosterone therapy does not increase the risk of prostate cancer but testosterone can be dangerous in men who develop prostate malignancy.
Men already on testosterone replacement therapy must be screened regularly for cancer of the prostate. This is why I believe only urologists should be prescribing testosterone therapy. Urologists are the experts in the early diagnosis of prostate cancer.
The PSA test is highly sensitive but not very specific for prostate cancer. DRE is highly dependent on physician experience. Urologists diagnose more prostate cancer by exam compared to any other medical specialty since the prostate is in their wheelhouse.
Using the PSA test to diagnose prostate malignancy is as much an art as it is a science. Understanding age related PSA differences, PSA velocity, PSA density and the hormonal influences on PSA levels are just a few of the complex diagnostic considerations urologists are equipped to interpret.
When PSA concerns arise, a urologist may order certain PSA derivatives to look more closely at the different types of PSA in the blood. If a urologist is concerned with the PSA results, a biopsy or MRI of the prostate will be the next step.
In some cases of elevated PSA development, urologists may hold testosterone therapy until prostate cancer is excluded. Men who are diagnosed with prostate cancer will be offered curative therapy in the form of radical prostatectomy or radiation. Many men diagnosed early will be cured of prostate cancer allowing them to resume testosterone replacement therapy with careful oncologic follow-up.

Venous Thromboembolism
Some studies have shown an increased risk of venous thromboembolism in men using testosterone therapy even when red blood cell count (hematocrit) is normal. Testosterone may have a pro-thrombotic effect on the platelets independent of it’s effect on blood viscosity by increasing red blood cell production.
Men on testosterone therapy should be warned regarding the signs and symptoms of venous thromboembolism so that prompt intervention can be employed. Venous thrombosis often presents with swelling, redness and pain of an extremity. Unusual presentations such as dark urine can occur if a clot forms in the renal or hepatic veins.
Men who develop a venous thrombosis require emergent evaluation and anticoagulation to prevent pulmonary embolism. Consultation with hematology is imperative to exclude hypercoagulable states. Testosterone cessation may be recommended along with blood thinner treatment until the clot is dissolved. Once the clot resolves, careful discussion between urology, hematology and the patient must ensue to decide if hormone replacement therapy can be safely resumed.
Heart Disease and Stroke
Some studies have suggested that men on testosterone replacement therapy are at increased risk for cardiovascular events including heart attack and stroke. While these studies were heavily criticized due to poor study design, the FDA put a black box warning on all testosterone products in 2014. This black box warning states that testosterone may increase the risks of clots, heart attack and stroke. It is found on the package insert of all FDA approved testosterone formulations.
Around the same time these concerning articles were published, the FDA approached testosterone drug manufacturers and told them to pony up the cash to fund a large randomized controlled trial to clarify the cardiovascular risk associated with testosterone usage. The Traverse trial was published in the New England Journal of Medicine in the summer of 2023. This was a large multi-center randomized placebo controlled study of over 5,000 men.

The Traverse findings revealed that testosterone therapy did NOT increase the risk of heart attack or stroke compared to placebo. This is a landmark study but it does not answer all of the questions surrounding the issue of cardiovascular risk. For example, the study was done using topical testosterone so we may not be able to extrapolate these results to other forms of testosterone therapy such as injections or oral testosterone.
The Traverse trial also found a slight increased risk of atrial fibrillation, venous thrombosis and kidney injury in men using testosterone.
When it comes to cardiovascular disease, I am always hesitant to start men on hormone replacement therapy if they have unstable cardiovascular or cerebrovascular disease. Careful discussion with cardiovascular medicine must take place in order to determine the feasibility of using testosterone in these men.
Men with a history of venous thromboembolism must also be approached cautiously and consultation with hematology is strongly recommended. In my experience, most hematologists are okay with these men being on testosterone therapy if they are properly treated without supraphysiologic testosterone dosing and maintained with a normal hematocrit.
Men with atrial fibrillation could potentially see an increase in atrial fibrillation episodes after starting testosterone therapy. This is sometimes difficult to tease out from other causes of atrial fibrillation exacerbation since so many factors can irritate the cardiac conduction system. However, I always discuss this issue with the patient’s cardiologist before starting any form of testosterone replacement therapy.
As with venous thromboembolism, I think it is very important to avoid supraphysiologic testosterone levels in men with atrial fibrillation. I also prefer to start at low doses of testosterone and gradually increase them into the mid-normal range of physiologic testosterone.
Mental Health Consequences of Low Testosterone & TRT
Testosterone passes through the blood brain barrier in support of normal brain function. Testosterone receptors are located in several parts of the brain including the cortex and hippocampus. There is no doubt that testosterone along with some of its metabolites play a role in normal mental health.
Low testosterone levels have been associated with a reduction in cognitive abilities. Cognitive functioning refers to multiple mental abilities including thinking, spatial memory, reasoning, verbal memory and decision making. A causative link between low testosterone and a decline in cognitive functions has yet to be determined although some potential mechanistic data in Alzheimer’s disease has been presented.

Male hypogonadism has also been associated with mood disorders including dysphoria, depression and anxiety in some studies. Other studies have not found a link between hypogonadism and depressive symptoms. Clinically, men taking testosterone generally report improvement in mood swings, motivation, sense of well being, sleep, self image and anxiety despite the conflicting literature.
Men with advanced prostate cancer are often treated with testosterone lowering drugs such as luteinizing hormone releasing hormone (LHRH) agonists. LHRH agonists reduce testosterone to castrate levels. These men often report adverse mental health issues such as dysphoria, irritability, listlessness and even suicidal ideation.
The Impact of Testosterone Deficiency on Quality of Life and Mood
Quality of life (QoL) is a conglomeration of psychological factors contributing to the subjective assessment of an individual that “life is good”. Quality of life is a multidimensional assessment of mental, physical and emotional health parameters.
Men with low testosterone levels typically report lower quality of life scores. Symptoms contributing to these lower QoL scores include fatigue, lack of motivation, irritability, dysphoria, mood swings, reduced sexual performance, cognitive impairment and even negative work performance.
Multiple randomized placebo controlled studies and meta-analyses have demonstrated improved QoL scores in hypogonadal patients treated with testosterone therapy. While not universal, men with lower testosterone values at the time of diagnosis experience more pronounced improvements in QoL measures.
I’ve been prescribing testosterone therapy for two decades and it has been readily apparent that testosterone treatment improves QoL and mood in the majority of men. These improvements are not subtle in most cases. About 1 in 4 men treated in my practice with testosterone replacement therapy will report life changing improvements to mood and quality of life. Half of men will report significant improvements and 1 in 4 men don’t see much in the form of QoL benefits.
Anabolic steroids have been linked to mood swings, depression and aggressive behaviors. If excess testosterone levels are obtained in men treated for low T, some of these same psychological changes could theoretically occur.
We must keep in mind that men using anabolic steroids are typically using 10-20 times the medically appropriate dose of testosterone along with other steroids and compounds that promote muscle mass such as insulin and growth hormone. However, men on medically prescribed testosterone replacement therapy should avoid supraphysiologic testosterone levels in most cases due to the theoretical risk of adverse mental health consequences and other side effects.
Men properly diagnosed and treated by a urologist for low testosterone almost never exhibit negative effects on mood or aggressive tendencies. I inform my patients that “roid rage” from medically appropriate dosing of testosterone therapy is a myth.
Testosterone Replacement Therapy and Anxiety
Low T symptoms may include generalized anxiety. Animal and human studies have shown that low testosterone levels are associated with anxiety and panic disorder. Both free and total testosterone levels have been inversely associated with generalized anxiety symptoms. CAG repeat polymorphism of the androgen receptor have also been implicated with anxiety in men.
While not extensively studied, testosterone supplementation seems to have an anxiolytic effect in men. In my clinical experience, men treated with testosterone replacement therapy do report improvements in anxiety and irritability. Testosterone’s central effects on the nervous system and serotonin pathways may explain it’s anxiolytic properties.
While the effects of testosterone are usually positive when it comes to anxiety, this generally applies to men with testosterone levels in the normal range. When men are treated with excess testosterone, anxiety can actually be worsened. This can occur in men treated medically to abnormally high testosterone levels as well as in men abusing anabolic steroids.
Anxiety symptoms can also be due to a bon a fide anxiety disorder unrelated to sex hormones. Men with severe anxiety symptoms should be referred for psychiatric consultation and not assumed to have low T related anxiety. Men with persistent anxiety after adequate testosterone supplementation should be referred to psychiatry as well for further evaluation and treatment.
Testosterone Therapy and Depression
Depressive symptoms can range from dysphoria to major depression affecting millions of men in the United States. Testosterone and some of it’s metabolic byproducts are neuroactive steroids that impact mood and behavior. Animal studies suggest that testosterone increases serotonin levels in the brain perhaps explaining it’s positive effect on depression. Many anti-depressant medications including SSRIs work by increasing serotonin levels.
Some studies have demonstrated that lower testosterone levels as well as alterations in the androgen receptor are associated with depressive symptoms in men including dysthymia, fatigue and anhedonia.
Most studies examining the effects of testosterone on depressive symptoms have shown improvement with testosterone therapy. In my clinical experience, testosterone replacement therapy usually has a very positive impact on mood and depressive symptoms. I’ve never seen a case where someone reported worsening depression after initiating treatment for hypogonadism.
Of course, depression can also coexist with low testosterone. Many of the symptoms of depression and low testosterone are shared by these two conditions which can make diagnosis tricky. Both depression and low testosterone can cause sadness, irritability, memory issues, insomnia and anhedonia.
The physical symptoms of depression and low testosterone tend to be different. Low testosterone is often associated with a loss of muscle mass and strength whereas this is not seen in depression. Men with low testosterone may also experience breast symptoms such as tenderness or gynecomastia as well as testicular atrophy, issues not seen in men with depression. Physical symptoms of depression may include headache and back pain which is not something we typically see in the low T patient.
Needless to say, distinguishing between depression and low testosterone can be challenging. Men who present with severe depressive symptoms or a history of depression should be referred to psychiatry. While testosterone therapy may help depressive symptoms, pharmacologic treatment or cognitive therapy may also be warranted in these men. Men with depressive symptoms that fail to respond to adequate testosterone replacement should also be referred for psychiatric consultation.
Some men with low testosterone present to my practice already on anti-depressant medication. After initiating testosterone replacement therapy some of these men see a dramatic improvement in depressive symptoms. This may allow them to lower the dose of their anti-depressant medication or stop it altogether. However, such pharmacologic maneuvers must be done in concert with close psychiatric follow-up.
Effects of High Testosterone on Mood
Most of the data regarding the effects of elevated testosterone levels on mood come from exogenous testosterone administration. Few studies have looked at high endogenous levels of testosterone and mood although some have suggested increased aggression and risk taking behavior.
One placebo controlled trial using high doses of injectable testosterone demonstrated an increase in anger and hostility after a few weeks of therapy. Much of the reported data on the impact of exogenous testosterone on mood unfortunately comes from the steroid abuser community.
Performance enhancing steroid use typically involves supraphysiologic testosterone dosing and has been shown to cause a variety of mood disorders including depression, irritability, hostile tendencies and mania. It is important to keep in mind that men abusing anabolic steroids tend to use multiple compounds, not simply high doses of testosterone cypionate or enanthate. In many cases, they also combine anabolic steroids with other medications including growth hormone, animal steroids, insulin and SARMs.
It’s not uncommon to see men using anabolic steroids develop depressive symptoms upon drug cessation. This could be due to the rebound hypogonadism caused by suppression of the hypothalamic-pituitary axis or though another mechanism.
Many of the adverse mental health consequences associated with performance enhancing steroid use have been assumed to occur in men treated with medically supervised testosterone therapy. This is simply untrue. Testosterone treatment for hypogonadism involves correcting testosterone levels into the normal range, not the supraphysiologic levels achieved during steroid use. These men will often achieve testosterone levels 20-50 times physiologic levels when using anabolic steroid compounds.
Testosterone Therapy and Aggression
As stated above, abusers of anabolic steroids can demonstrate mood disorders including tendencies towards aggression and risk taking behaviors. There is no good scientific evidence that medical treatment of hypogonadism using testosterone leads to aggression or threatening behavior.
Conclusions
Testosterone deficiency has been associated with adverse mental health consequences including impaired cognitive abilities, depressive symptoms, reduced quality of life scores and anxiety. Testosterone and it’s metabolites clearly impact the nervous system in important ways.
Hormone replacement therapy using FDA approved medications to treat hypogonadism has been shown in most studies to benefit mental health. Men on testosterone therapy typically report improved mood, reduced anxiety, cognitive benefits and improvement in overall quality of life scores.
Testosterone injections are a viable and often the preferred form of testosterone replacement. These drugs also lead to improved mental health in most men as long as they are used appropriately.
Mental health issues such as depression and anxiety can coexist with hypogonadism. Consultation with urology and psychiatry is preferred so a multidisciplinary approach to care can be implemented.
