Testosterone Production
Men produce both “male” and “female” hormones important for normal male physiology. The quintessential male hormone is testosterone and testosterone is by far the most important androgen in the body. Other androgens such as androstenedione and DHEA are not major players in the hormone therapy field.
Testosterone production is mediated by the Leydig cells of the testicle. The Leydig cells are under the control of the pituitary gland, the “master” gland that sits at the base of the brain. The pituitary gland produces a hormone called LH or luteinizing hormone that travels to the testicles and acts on the Leydig cells to stimulate testosterone production.
Another hormone called FSH or follicle stimulating hormone is also produced by the pituitary gland. FSH works on the Sertoli cells of the testicle to promote healthy sperm production and sperm quality. Testosterone production in the testicle is also very important for normal sperm manufacturing, a process called spermatogenesis.
As the Leydig cells increase testosterone production, the androgen can enter the blood stream. Some of the testosterone is bound to proteins while some testosterone remains unbound or free. Only about 2% of the total testosterone is unbound but some of the protein bound testosterone is loosely bound to albumin making bioavailable. Bioavailable testosterone is the portion of total testosterone that is available to the tissues and consists of free testosterone plus testosterone loosely bound to proteins in the blood.
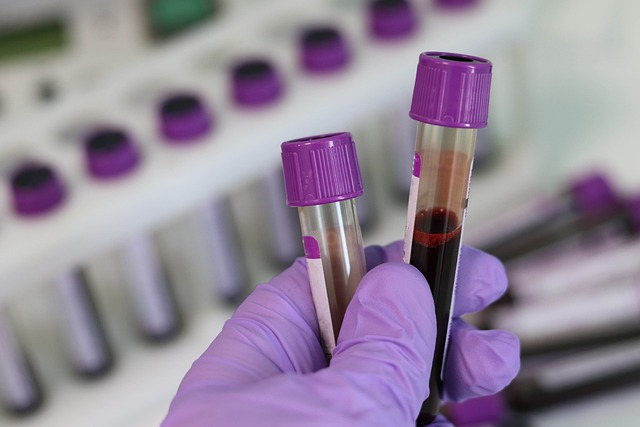
Both total and free testosterone levels can be measured in the blood. Testosterone must leave the blood stream and enter the organs and tissues to exert its powerful effects. If testosterone is tightly bound by a protein called sex hormone binding globulin or SHBG it becomes trapped in the blood stream where it can’t alter physiology.
Once testosterone enters the tissue of interest it enters the cell and bind to the androgen receptor. Testosterone is the main androgen in the body. The testosterone/androgen receptor complex can then enter the nucleus of the cell and alter the transcription of genes. Proteins are generated from this gene activation and these proteins can alter the function of cells, tissues and organs.
A small amount of testosterone is converted to estradiol by aromatase, an enzyme located in fat cells. Estradiol also travels via the blood stream and needs to bind to estrogen receptors in order to exert it’s hormonal effects.
A small percentage of testosterone is also converted into another hormone called DHT or dihydrotestosterone. DHT is a very powerful androgen but exerts its effects mainly in the prostate and hair follicles. Increased DHT levels can accelerate male pattern baldness in men taking testosterone and it may also stimulate prostate growth. 5-alpha reductase is the enzyme that converts testosterone into DHT. This enzyme can be inhibited by the drugs finasteride and dutasteride.
Testosterone Therapy and Estrogen Levels in Men
When testosterone levels decline in men they can develop symptoms such as low sexual desire, poor sexual function, fatigue, insomnia, depression, weight gain and difficulty building muscle mass. Testosterone therapy involves the correction of low testosterone levels in men by the administration of testosterone.
Exogenous testosterone can be given in different forms including topical gels, oral pills, injections and implantable testosterone pellets. Other drugs called selective estrogen receptor modulators are sometimes used to treat low testosterone. The most common of the selective estrogen receptor modulators used to treat low testosterone is clomiphene citrate.
Selective estrogen receptor modulators like clomiphene citrate block the estrogen receptor at the level of the pituitary gland. This blocks the negative feedback that estradiol exerts on the pituitary resulting in increased production of LH, FSH and testosterone.
Correction of testosterone deficiency with testosterone replacement therapy can lead to improvement in sexual function, energy, mood, concentration, sleep, bone mineral density and body composition. It can also help promote healthy weight loss.
Testosterone replacement therapy can also cause side effects including acne, fluid retention, high blood pressure, male infertility, worsening sleep apnea, blood clots, erythrocytosis and gynecomastia. Testosterone therapy is generally contraindicated in men with prostate cancer or breast cancer. Prostate and breast cancer cells can be stimulated by increasing testosterone.
Men on testosterone therapy must be carefully monitored by an expert physician. Monitoring should include a physical examination every 6-12 months. Examination should include the testicles, breast and prostate. Blood pressure needs to be monitored and lab checks are typically done every 3-4 months. Lab testing should include testosterone, estradiol, PSA and hematocrit. I also like to monitor metabolic health and lipid profiles annually.
When testosterone is prescribed elevated estrogen levels may develop due to a process called aromatization. This is expected due to the presence of aromatase, an enzyme that converts testosterone into estradiol, the primary estrogen in men. The aromatase enzyme is primarily located in adipose tissue, aka fat tissue. Obese males tend to have higher aromatase activity and may be more prone to elevated estrogen levels when being treated for low testosterone.
Historically, estrogen was considered primarily a “female hormone” while testosterone was viewed as the quintessential male hormone. However, this view has changed based on science and we now know that estrogens are important for men. They are quite vital for erectile function, mood, bone mineral density and even muscle mass. Estrogen receptors are located in a variety of tissues within the male body including the penis, brain, bones, fat cells and muscle. So adult males on hormone therapy need to manage estrogen levels effectively because estrogen plays a key role in male physiology.
Estrogen also serves as a negative feedback hormone by binding to estrogen receptors in the pituitary gland to modulate the production of luteinizing hormone.
Testosterone Replacement Therapy and Estradiol Balance
Since it is abundantly clear that both testosterone and estrogen are important for men’s health we need to maintain the correct balance of these hormones when treating men with testosterone deficiency. My target when treating men with testosterone replacement therapy is to increase testosterone levels into the top quartile of normal (700-1,000 ng/dL).
Mildly elevated estrogen levels are expected when I begin testosterone replacement therapy. There is NO reason to automatically put men on an aromatase inhibitor when they start hormone therapy. Any physician who suggests doing so, lacks training and expertise in the field of andrology. And just for the record, the only specialists in medicine who are considered experts in andrology are urologists and endocrinologists. Urologists are also the sexual medicine experts.
Some of the benefits of testosterone replacement therapy are actually driven by the rise in estrogen levels seen on therapy. So, it’s not just about raising testosterone levels in men with testosterone deficiency, estrogens also matter as men age. To be clear, we want to see a rise in both serum testosterone levels and estradiol after starting someone on testosterone therapy. But, we do like to see a proper balance of these two sex hormones maintained or adverse effects can develop.
Ideally, we like to see a testosterone to estradiol ratio of 10:1. So, a testosterone of 800 ng/dL with an estradiol of 52 pg/mL would be great. Normal estradiol levels are typically between 12-42 pg/mL so a 52 pg/mL reading is slightly elevated. But, that’s OK and generally preferred in my practice. Those estrogens are important and likely drive some of the clinical benefits experienced by men taking testosterone.
Now if testosterone is 800 ng/dL and estradiol is 100 pg/mL the ratio is less than 10:1 and adverse effects may arise. This is not a great ratio because of too much estrogens so treatment to bring down the estradiol level may be warranted in my practice, generally through aromatase inhibition.

Differences in Aromatase Activity in Men
Aromatase is an enzyme predominantly located in the adipose tissue or fat stores of the body. Men with more adiposity tend to have more estrogen production due to higher aromatase activity but this is not always the case. There may also be individual differences in enzyme activity that can lead to differences in estradiol levels in men on testosterone therapy.
Generally, men with more belly fat tend to have higher estradiol levels while treated with testosterone but there are exceptions to this general rule. Weight loss can lower estradiol levels. It’s important to follow estradiol levels in men after starting testosterone treatment in order to recognize estradiol excess and low testosterone to estradiol ratios that may result in adverse effects or poor clinical results. When estrogen levels become a problem, aromatase inhibition is often the solution
Due to the individual differences in aromatase activity in men, therapy for high estrogen levels must be individualized. There is no one size fits all solution in hormone therapy so beware of cookie cutter approaches by non-expert physicians.
Patients don’t always follow the textbook. I had one patient in my sexual medicine practice who defied all the textbooks. He was a thin healthy 60 year male on testosterone cypionate 125 mg weekly. Testosterone levels were 800 ng/dL but after 6 months of therapy his estradiol level rose to 500 pg/mL, the highest value I have ever seen. Estrogen production was so abnormal that I began a search for an estrogen secreting tumor which thankfully I didn’t find. Certain cancer cells can secrete estrogen.
Once I excluded malignant pathology I began a low dose of an aromatase inhibitor and his estradiol came down to 50 pg/mL. Sexual function improved and more testosterone resulted from the aromatase inhibition.
Side Effects of Estrogen Excess or Abnormal T:E ratio
When estradiol levels are markedly elevated or the testosterone to estradiol ratio drops below 10, some men may experience an increased risk of side effects including mood disorders, erectile dysfunction, edema, weight gain, difficulty losing body fat and breast enlargement. If high estradiol levels go unchecked in a male patient complaining of breast sensitivity or pain they can develop male breast enlargement, a condition called gynecomastia. Gynecomastia is a serious problem because once the breast tissue develops it requires surgical removal.
In some cases, men will experience great results after starting testosterone replacement therapy only to see those results dissipate 4-6 months later. Sometimes this is due to rising estradiol levels that simply develop over time. These patients may not complain of specific estradiol related side effects such as breast tenderness, they just aren’t seeing the clinical benefits they were experiencing earlier in their treatment course.
Restoring the testosterone to estradiol balance with medication can easily eliminate the side effects of estradiol excess and prevent devastating complications such as gynecomastia. So, there is no need to start someone on an aromatase inhibitor when they begin testosterone therapy but you must carefully monitor their estradiol levels and periodically ask them about possible estrogen related side effects.
Urologists understand andrology better than any medical specialty which is why we only have urologists at my practice. When we initially diagnose patients we take an exhaustive medical history and perform a thorough physical examination. A careful assessment of erectile function must be made. A formidable laboratory investigation will follow to include assessment of male and female hormones as well as pituitary hormones.
If too little testosterone is being produced by the male body we will try to find the underlying cause. Medical issues such as thyroid dysfunction, pituitary tumors and iron storage diseases can cause reduced testosterone levels. Some medications can impair testosterone production.
When to Take Anastrazole with Testosterone
When men complain of poor results from testosterone therapy or specific side effects indicative of high estradiol levels a thoughtful discussion must ensue. Estrogen and testosterone levels need to be carefully assessed.
If testosterone and estrogen levels are both elevated, a simple dose reduction in testosterone therapy may solve the issue and restore the proper balance between these two essential hormones. Encouraging men to lose body fat will also help lower estradiol levels by reducing aromatase activity in the body.
Most commonly an aromatase inhibitor will be prescribed to restore the balance between testosterone levels and estrogen. Aromatase inhibitors are oral medications that block the aromatase enzyme. They were developed and are still used to treat estrogen receptor positive breast cancer. But they can also be used to block aromatase in men on testosterone. This essentially interrupts the conversion of testosterone into estradiol. Estradiol levels should fall and testosterone levels should rise.
Aromatase inhibitors are generally taken with a frequency anywhere from a few times a week to daily, depending on clinical parameters. The goal is to restore the T:E ratio to 10 or greater, not necessarily normalize estradiol levels in our practice.
Remember, estrogen plays some key roles in male physiology. Some of the benefits of testosterone therapy likely come from modestly elevated estradiol levels. So, our goal is to restore the T:E ratio and tailor treatment to optimize clinical benefits. We generally don’t want to lower estradiol too much because this can have detrimental effects.

Consequences of Low Estrogen Levels in Men
Far too often, men treated by non-expert physicians for low testosterone are automatically started on an aromatase inhibitor when they start testosterone therapy. This will often take their estradiol levels down to low normal or even very low levels. If estrogen is important for men, why would they do this? Because they simply don’t understand andrology or hormone replacement therapy.
When estradiol levels are too low, men are at risk for adverse health effects including osteoporosis, erectile dysfunction, depression and possibly poor vascular health. Believe it or not, I’ve seen men suffering from the same symptoms women experience during menopause when they are taking too much of an aromatase inhibitor. They can get fatigue, hot flashes, low libido and depression. Men can also experience erectile dysfunction, low libido and ejaculatory dysfunction when over treated with aromatase inhibitors.
In one case, I actually saw a 55 year old man with osteoporosis who had been on high dose aromatase inhibition for years prescribed by an online testosterone clinic. They drove his estradiol levels to almost nothing and told him that would help him burn more fat. Fortunately we stopped aromatase inhibitors to allow estrogen production once again. Improved estrogen levels eventually improved his bone density, reversing the osteoporosis.
In summary and in layman’s terms, I tell my patients that when estrogen levels are too high it can be bad. But when they are too low, it can be very bad. The same logic applies to testosterone levels.
Taking Anastrozole with Testosterone
When taking aromatase inhibitors, hormone levels should be monitored during treatment. More importantly, you should be talking to your urologist or endocrinologist regularly regarding your clinical results and possible side effects. That includes adverse effects that may be related to high estradiol levels. If you are on hormone therapy and not meeting with a qualified physician regularly to discuss treatment results and potential side effects, find a new doctor.
If you experience poor clinical results or estrogenic side effects your physician will review your current and previous hormone levels. If estradiol levels are elevated and the ratio of testosterone to estradiol is less than 10:1 it’s probably time to start anastrozole or similar aromatase inhibitor. Typically low dose anastrozole will resolve the issue. Only in rare cases will high dose therapy be required.
Hormone levels should be carefully monitored after starting anastrozole. Typically, anastrozole will increase testosterone and decrease estradiol levels with the goal of restoring a 10:1 or greater testosterone to estradiol ratio. Individual differences exist and some men are more sensitive to hormones than others therefore a personalized evidence based approach is what I use.

How to Take Anastrozole with Testosterone
The most common treatment for low testosterone is exogenous testosterone injections. While there are other treatment options that men should consider, testosterone injections take the pole position. Testosterone replacement therapy using injectable testosterone can be done with either testosterone cypionate or testosterone enanthate. Intramuscular and subcutaneous injections are both acceptable methods.
Men wishing to father children should not be treated with exogenous testosterone. Drugs like clomiphene citrate or human chorionic gonadotropin (HCG) can be used to treat low testosterone in men wishing to preserve their fertility potential.
Testosterone injections can be done either subcutaneously, similar to insulin injections or intramuscularly. The frequency of administration is 1-2 times weekly. Other treatment options for low testosterone include topical gels, oral testosterone pills and implantable testosterone pellets. Testosterone injections are by far the most popular treatment, mainly due to cost. Injections are quite affordable, even when not covered by insurance.
When adding aromatase inhibitors to the treatment regimen I usually start with low dose anastrozole. Typically this will be 0.5 mg two to three times weekly. If performing injections twice a week men will often take their anastrozole the day of or day after an injection.
Careful monitoring of hormone levels will follow along with clinical assessment of adverse effects and clinical benefits. I usually assess testosterone and estradiol levels about one month after starting aromatase inhibitors. If dosing adjustments are required I will repeat lab testing every 4-6 weeks until I get hormones optimized. Once optimization is achieved lab testing can be performed every 3-4 months to assess biomarkers including PSA, an important screening test for prostate cancer.
The dose of aromatase inhibitors may need to be adjusted based on hormone levels. Testosterone replacement therapy may also require a dose adjustment if testosterone levels increase too much.
Side Effects of Aromatase Inhibitors
Anastrozole and other aromatase inhibitors are generally well tolerated medications. However, like all drugs, they can cause side effects including hot flashes, GI upset, low libido, joint pain and depression. Usually, side effects can be managed with a dose reduction or change to a different aromatase inhibitor.
Estrogen production plays a vital role in male physiology so lowering them too much can make men feel like postmenopausal women. Symptoms can include depression, sexual dysfunction and fatigue. Really low female hormone levels can also effect bone density and cause an increased risk of cardiovascular disease.
Men started on aromatase inhibitors must be closely monitored for side effects. Testosterone can also cause increased risk of blood clots, high blood pressure and increases in PSA. Hormone therapy requires a precise diagnosis and very careful follow-up to mitigate the risks of side effects and medical

In Summary
Testosterone deficiency is a serious condition in men where more testosterone is needed to enable normal physiology. Men with testosterone deficiency can suffer from a variety of symptoms and be at increased risk for certain health conditions including diabetes and metabolic syndrome. The diagnosis of testosterone deficiency or hypogonadism requires a meticulous assessment by an expert physician, preferably a urologist.
If there are no medical contraindications to hormone replacement therapy, testosterone can be prescribed. The most common drug used to treat hypogonadism in men is injectable testosterone but other viable treatment solutions are available. Men wishing to father children should not be treated with exogenous testosterone and will be better served by using drugs such as clomiphene and HCG, both of which increase endogenous testosterone production.
Regardless of chosen drug therapy for low testosterone, men require close follow-up with a qualified physician. Follow-up must include a careful clinical history and review of potential side effects as well as a comprehensive physical examination. Breast and prostate masses must be excluded as part of that exam and blood pressure should also be monitored. Lab testing is required periodically to assess hormone levels, PSA, hematocrit, lipid profile and blood sugar.
Some men on testosterone therapy will see estrogen levels rise and this is not necessarily a bad thing. Estrogens can be good in men and some of the benefits from testosterone therapy actually come from higher estrogens. But too much estrogen or an imbalance between testosterone and estrogen can be detrimental and lead to poor results, side effects and even adverse health outcomes.
Careful assessment of clinical outcomes and hormone levels with blood testing will identify men who may benefit from additional hormone manipulation. When estrogens are too high, the most common solution is the administration of an aromatase inhibitor. Aromatase inhibitors block the conversion of testosterone into estradiol and when properly used, restore the normal balance of these hormones.
Like all drugs, aromatase inhibitors can cause side effects, so careful monitoring by an expert urologist cannot be overstressed.

